Carcinoma
The Common Vein Copyright 2008
Definition
Esophageal cancer is a malignant growth disorder of esophageal mucosa. Historically squamous cell cancer was the predominant type; however, more recently, a surge in adenocarcinoma as the more common entity has evolved. Sqaumous cell carcinoma characteristically occurs in the thoracic esophagus while adenocarcinoma occurs at the GE junction.
Many different causative factors have been associated with this condition including GERD, Barrett’s esophagus, dietary factors, smoking and geographic location.
The disease results in an aggressive space occupying mass that progressively impinges on the lumen of the esophagus to cause dysphagia
It is most commonly diagnosed by endoscopy and biopsy, staged with CT and PET scan, and best treated with a combination of surgical and medical therapies.
The overall prognosis is quite poor, with 5 year survival estimated to be between 10-13% for advanced disease. With the increased diagnosis of Barrett’s esophagus, and the routine surveillance that follows, earlier detection of cancer allows for treatment and better survival rates. Survival rates are much improved with more superficial cancers that are found with increasing frequency during endoscopic surveillance.
.
  Ulcerating Squamous Cell Carcinoma of the Esophagus Ulcerating Squamous Cell Carcinoma of the Esophagus |
| 02425 02420 code esophagus + mass narrowing stricture ulceration heaped edges squamous cell carcinoma + grosspathology |
| Ulcerating Esophageal Carcinoma with Heaped Edges |
| 01270c code esophagus + fx mass + dx carcinoma + barium swallow upper GI UGI imaging radiology contrast X-Ray mass neoplasm malignant primary carcinoma cancer tumor Courtesy Ashley Davidoff MD |
Causes and Predisposing Factors
ie etiology and pathogenesis
Squamous cell carcinoma and adenocarcinoma each have their own predisposing conditions, and as such, will be described separately.
Causes Related to Squamous Cell Carcinoma:
Geographic location has been shown to be a risk factor for the development of squamous cell carcinoma of the esophagus. Asian countries have a higher incidence than that of the western part of the world.
Dietary risk factors also exist. Much like that of other gastrointestinal cancers, foods with n-nitroso compounds are thought to increase the risk. Within the Asian countries, the common practice of chewing of the Betel nut, has been associated with squamous cell carcinoma.
Other dietary risk factors include the consumption of alcohol. A correlation between the amount consumed and the risk of cancer exists.
Tobacco use has also been closely associated with squamous cell esophageal cancer.
Patients with underlying conditions that affect the esophagus are also at increased risk. A previous history of caustic ingestion, classically with lye, increases the risk.
Causes Related to Adenocarcinoma:
The most important risk factor for the development of adenocarcinoma of the esophagus is a history of Barrett’s esophagus. The progression of Barrett’s to carcinoma is well documented and reviewed at length in the section on Barrett’s.
Other risk factors for the development of adenocarcinoma of the esophagus include tobacco use, obesity, GERD, and other conditions that will increase acid exposure in the esophagus
Statistics
In the USA it is relatively uncommon with about 10,000 new cases per year or between 2 – 8 people per 100,000
There are certain areas in China with 100 new cases per 100,000
Race
Higher in the black population – could this show a genetic predisposition?
Sex
M:F range from
2:1 to 20:1.
Age
adult disease
usually over age 50
Other Statistics
1% of all cancers
10% of gastrointestinal malignancies
Result
Since the lymphatic network in the submucosa is so allows both circumferential and longitudinal spread and the disease is usually more extensive than the macrsosopic appearance and early lymphatic spread to areas remote from main mass is characteristic. As mentioned above, the 5 year survival rates for esophageal cancer are quite low. Early detection is important as if found prior to metastasis, the treatment options are more plentiful.
Gross Pathology
polypoid or fungating (common)
ulcerating form
infiltrating form
varicoid form
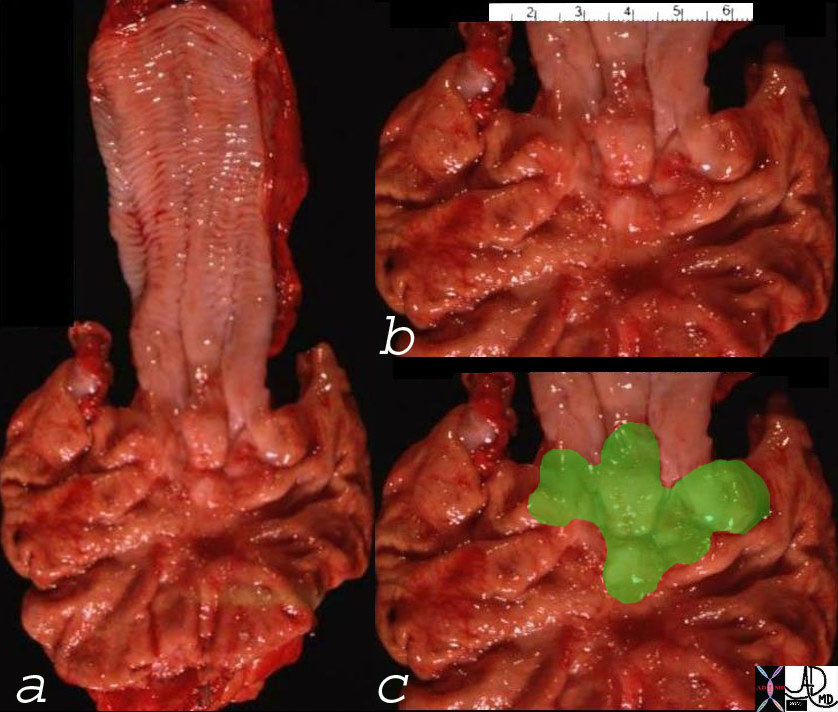 Ill Defined GE Junction Tumor – Adenocarcinoma Ill Defined GE Junction Tumor – Adenocarcinoma |
| 00567c03 distal esophagus GE junction gastroesophageal junction stomach GE junction tumor fx nodular appearance to the GE junction dx adenocarcinoma of the GE junction grosspathology malignant cancer Courtesy Ashley Davidoff MD |
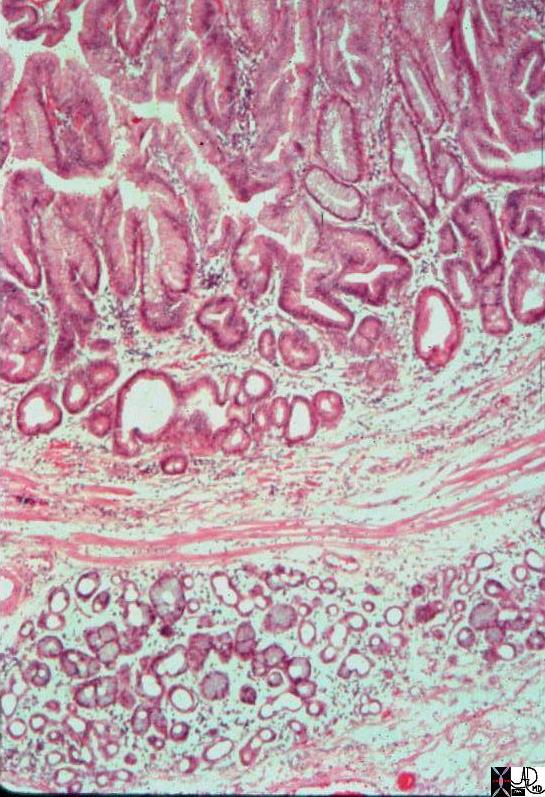
Histopath
squamous cell carcinoma (95%) Squamous cell carcinomas are moderately to well differentiatedsquamous cell carcinoma (common)
adenocarcinoma (4%)
Barrett 70%
GE junction 30%
other
adenoid cystic carcinoma
carcinosarcoma
Squamous cell carcinomas are moderately to well differentiatedsquamous cell carcinoma (common)
They pesent as;
well differentiated (common)
mderately differentiated (common)
poorly differentiated
Complications
The mass may cause local obstruction. Local extension into mediastinal structures is early and common. Tracheoesophageal fistula can occur in 5 -10%. Other complications include ulceration, bleeding airway compression, and invasion into the aorta. Systemic complications are characterized by metatastasis to nodes, lung, liver, adrenal gland.
Classification based on Staging
TNM system:
T, tumor <5 cm in length without circumferential involvement
T2 tumor >5 cm in length / circumferential or obstructive lesion
T3 extraesophageal spread
classification based on radiologic appearance
Diagnosis
Clinical
Clinically, patients present with a myriad of complaints, the most common of which is dysphagia. As the lumen narrows for the growth of the lesion, food is unable to pass smoothly thru the esophagus. Patients can present with upper gastrointestinal bleeding, weight loss, halitosis, in addition to many non-specific complaints.
The onset of the dysphagia is insidious. The esophagus is a pliable and mobile organ and is therefore forgiving and can accomodate the advancing mass. Thus clinical presentation and the onset of dysphagia is late.The delay in time to clinical presentation implies advanced disease at presentation and this affects outcome.
Imaging
With clinical suspicion, most patients undergo an upper endoscopy to evaluate the symptoms. This modality allows for direct visualization of the lesion and for biopsy for tissue diagnosis.
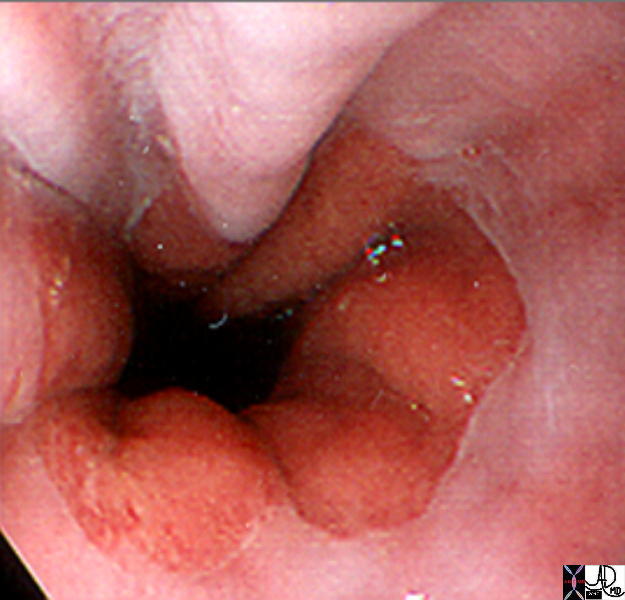
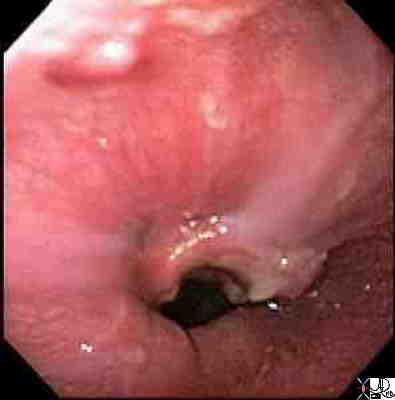 Carcinoma of the Esophagus Carcinoma of the Esophagus |
| 73940.400 73941.400 esophagus distal mass ulcerating bleeding carcinoma of the esophagus endoscopy endoscopic view Courtesy Joshua Namias MD |
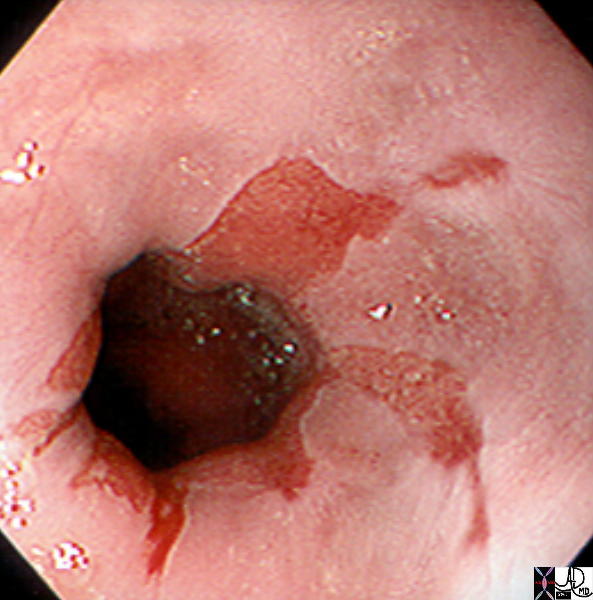
 Carcinoma of the Esophagus Carcinoma of the Esophagus |
| 73941.400 73941.400 esophagus distal mass ulcerating bleeding carcinoma of the esophagus endoscopy endoscopic view Courtesy Joshua Namias MD |
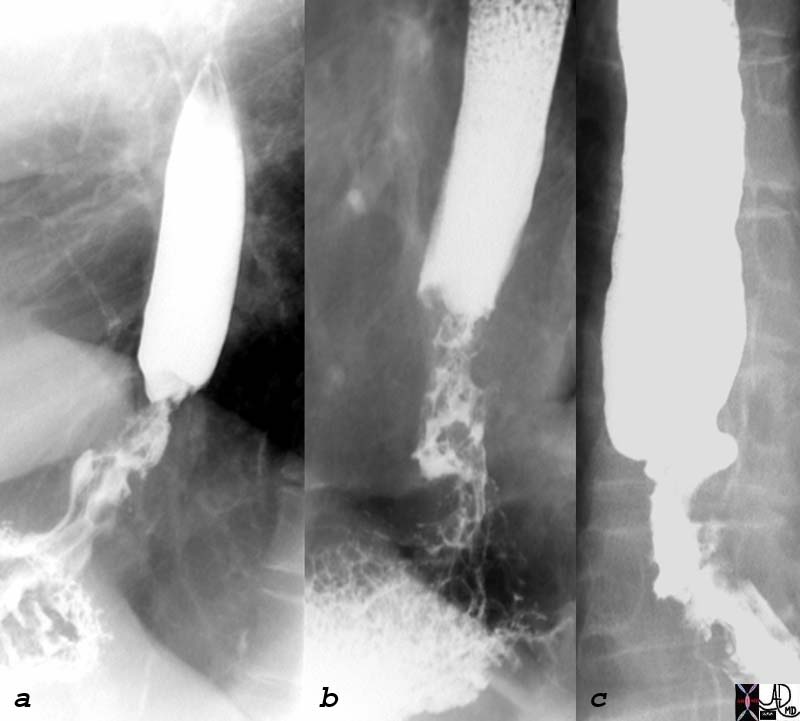 Irregular Distal Esophagus with Stricture – Adenocarcinoma of the GE junction Irregular Distal Esophagus with Stricture – Adenocarcinoma of the GE junction |
| 75711c01 dysphagia esophagus distal irregular stricture dx adenocarcinoma of the esophagus barium swallow Courtesy Ashley Davidoff MD |
 Long Relatively Smooth Malignant Stricture Long Relatively Smooth Malignant Stricture |
| Courtesy Ashley Davidoff MD 01240 esophagus + fx irregular stricture + dx carcinoma + barium swallow upper GI UGI imaging radiology contrast X-Ray mass neoplasm malignant primary carcinoma cancer tumor |

Long Mid Esophagus Malignant Stricture |
| Courtesy Ashley Davidoff MD 01246 code esophagus + fx irregular + fx long fx narrowed + dx squamous cell carcinoma + barium swallow upper GI UGI imaging radiology contrast X-Ray mass neoplasm malignant primary carcinoma cancer tumor |
Depending on the initial complaint, a barium study may also be performed.
Findigs may include a polypoid or fungating form, ulcerating form, or infiltrating form. If ulcerated a filling defect would be apparent, anf if it involves the esophagus ircumferentially an apple core lesion or a focal narrowing will be present. Once the diameter of the lumen becomes less than 13mm partial obstruction occrs, the lumen becomes functionally compromised the proximal esophagus dilates and dysphagia ensues.Any mucosal irregularity that raises uspicion should be evaluated an biopsied as dwcided by the endoscopist at the tine.
CT shows wall thickening anf the relationship to
mediastinal structures. Ominous signs iclude 1oss of fat planes invasion into trachea, aorta, pericardium, and distant metastases
Once a lesion is found, further diagnostic studies are often performed. Endoscopic ultrasound allows for great definition of the extent of the disease. This modality allows for visualization of the layers of the esophagus, such that the level of invasion can be identified. Biopsies of involved tissue and nodes can be performed.
CT scan allows for evaluation for metastatic disease as well.
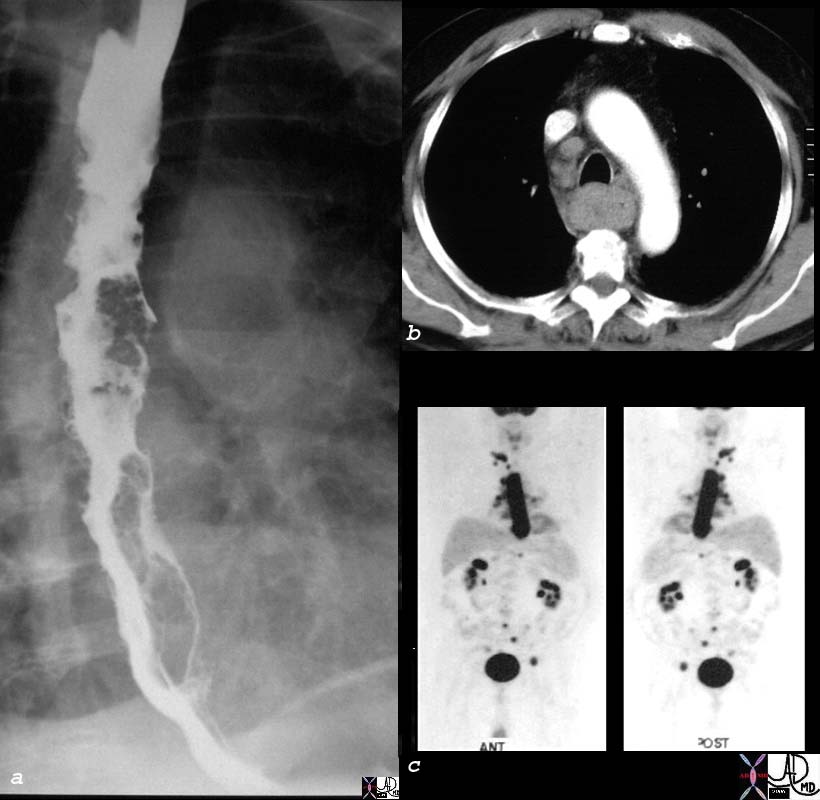 Staging by Non Invasive Method Staging by Non Invasive Method |
| 29885c03 esophagus lymph nodes primary esophageal carcinoma probably squamous carcinoma metastases to lymph nodes mediastinal lymphadenopathy mediastinum irregular lumen long segment single contrast bariu swallow CTscan PET scan NM Courtesy Ashley Davidoff MD |
Treatment
Treatment of esophageal cancer greatly depends on the staging of the disease.
If the tumor is localized to the esophagus, without evidence of direct or metastatic spread, surgery provides a cure. Typically an esophagectomy with gastric pull up is the treatment of choice. Mucosal resections, photodynamic therapies, and ablative techniques can be entertained.
If the disease is not resectable at the time of diagnosis, chemotherapy, often in combination with radiation therapy is undertaken.
 Stent in the Distal Esophagus Stent in the Distal Esophagus |
| 18203c esophagus carcinoma stricture tube stent dilatation treatment Courtesy Ashley Davidoff MD |

Gastric Pull Through |
| 76384 esophagus carcinoma cancer gastric pull through surgery treatment differential diagnosis dd dilated esophagus barium swallow Courtesy Ashley Davidoff MD 76386c01 |
Prognosis
3 – 75% 5-year survival rate
For superficial superficial esophageal carcinoma 5-year survival rate is 75% and for advanced lesions 5-25% 5-year survival rate. The presence of involved Iymph node metastases at the time of resection reduces the 5 year survival.

 Barretts Esophagus
Barretts Esophagus Barrett’s Esophagus
Barrett’s Esophagus Barret’s Esophagus by Endoscopy No Specific Findings
Barret’s Esophagus by Endoscopy No Specific Findings