Introduction
Pancreatic carcinoma is an aggressive malignant disease with a very poor prognosis. It is one of the more common malignancies that affect the American population, and accounts for about 30,000 deaths in America per year. It has an increased incidence in industrialized and Western cultures and is more common in men, usually occurring over the age of 60 (80%) It appears that chronic pancreatitis, diabetes and smoking are predisposing factors. 90% of the carcinomas arise from the epithelial cells of the exocrine pancreas. The disease is characterized by desmoplastic behavior so that it invades and encases neighboring vital structures early.
In most instances by the time the patient becomes symptomatic the disease is inoperable, and the patients usually succumb to the disease within a year of diagnosis.
Approach in the asymptomatic patient
If we are going to play any role in making a difference in this disease, early diagnosis, before involvement of other organs, is a key challenge. Unfortunately finding a small curable carcinoma is a rare occurrence and most the time we are left with a disease that has advanced too far for effective cure. Nevertheless our focus when reviewing the pancreas in any abdominal CT should be on the head and uncinate process because about 70% of pancreatic carcinomas arise from this part of the pancreas. Since the carcinoma is characteristically hypovascular, we should therefore be looking for a small hypodense rascal in the head of the pancreas. This is not to say of course suggesting that you should not look elsewhere but a focus using probability of finding disease is recommended. You will only find what you look for and so an active mind with a preconceived notion will sometimes yield remarkable results. Our search unfortunately is made more difficult and confounding by a few normal structures that reside in the region, including prominent ducts of the uncinate, and the bile duct itself.
In the following case the subtle nature of pancreatic cancer is noted.
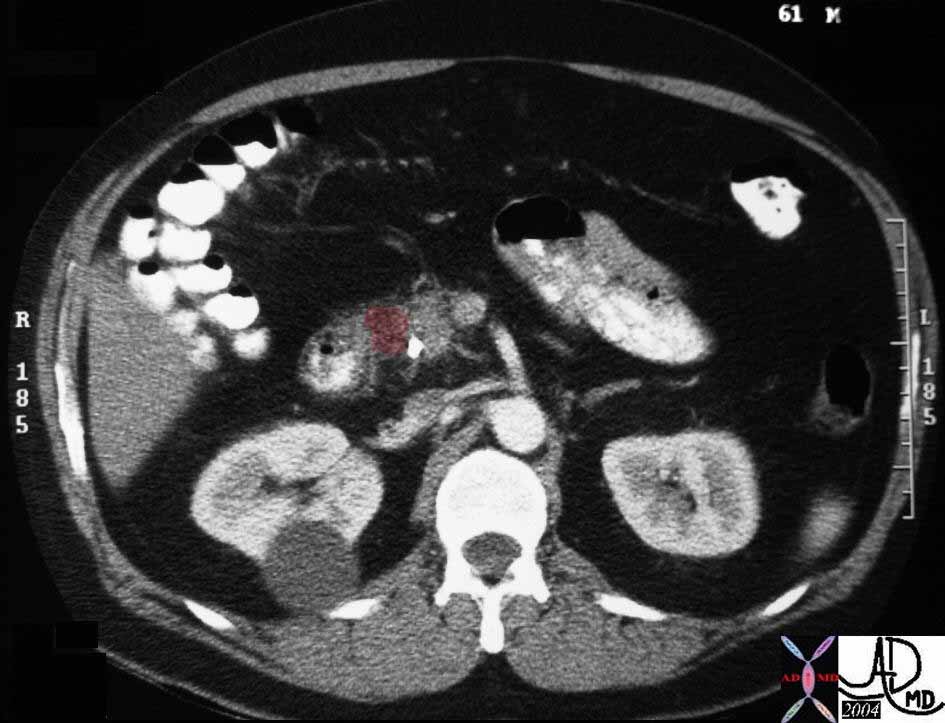
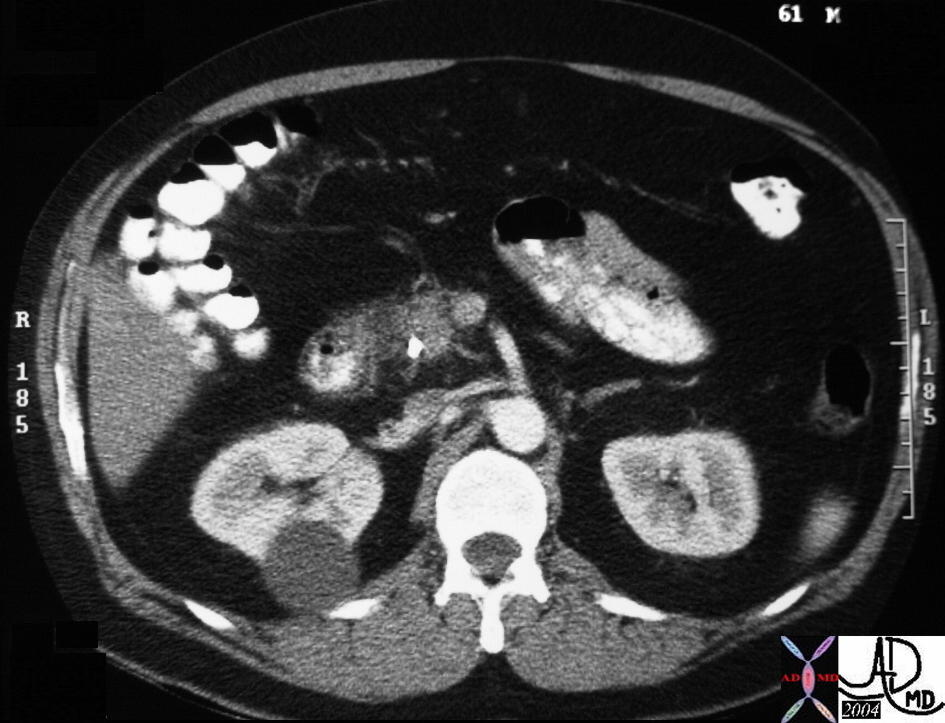
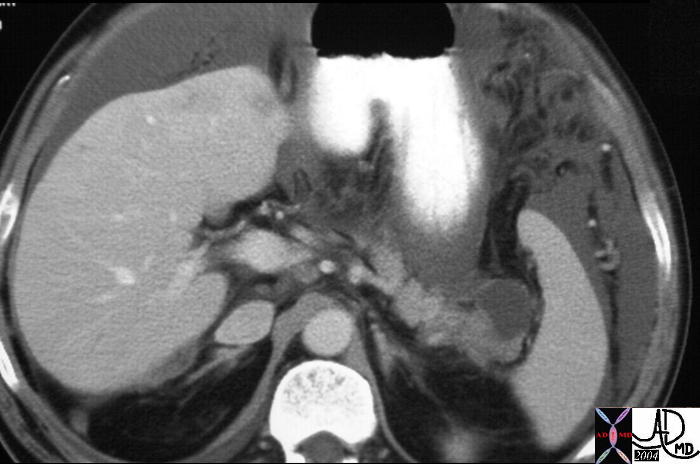
This is a 61 year old male who presented with painless obstructive jaundice and required a stent to relieve the obstruction. On review of the CT scan a subtle hypodense hypovascular mass was noted. Can you see the mass? It is lateral to stent and is just over 1 cms. in diameter. At this stage we are probably too late in our diagnosis for cure. 29970 Courtesy Ashley Davidoff MD
This is a 61 year old male who presented with painless obstructive jaundice and required a stent to relieve the obstruction. On review of the CT scan a subtle hypodense hypovascular mass was noted. In this image the mass is overlaid in maroon. 29970b Courtesy Ashley Davidoff MD
The following case deserves showing to expand on the importance of the analyzing the component parts of the head of the pancreas and the importance of following the pancreatic duct and the bile duct individually to their confluence. Any extra hypodensities must be explained, and heightened sensitivity must be maintained even for the most subtle of changes.
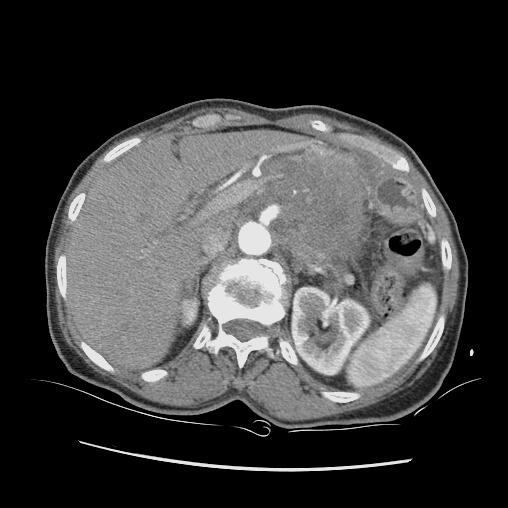
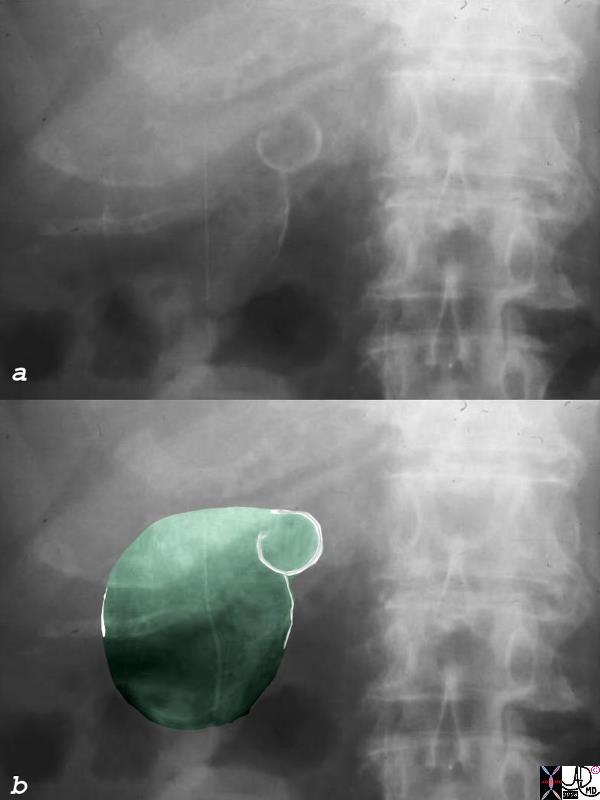
In this CTscan of the abdomen we identify a rounding out of the head and uncinate process with two hypodense components. Associated finding include a dilated gallbladder and a suggestion of intrahepatic bile duct dilatation. Our suspicion on this single image is of pancreatic carcinoma, but how do we interpret the findings in the head? We know that we should have at least two normal hypodensities in this region (bile duct and pancreatic duct), and we also know there is a hypodense mass lurking. The need to review all the images is wanting. 40839 Courtesy Ashley Davidoff MD
The
References
The
MCQ
The
Introduction
Pancreatic carcinoma is an aggressive malignant disease with a very poor prognosis. It is one of the more common malignancies that affect the American population, and accounts for about 30,000 deaths in America per year. It has an increased incidence in industrialized and Western cultures and is more common in men, usually occurring over the age of 60 (80%) It appears that chronic pancreatitis, diabetes and smoking are predisposing factors. 90% of the carcinomas arise from the epithelial cells of the exocrine pancreas. The disease is characterized by desmoplastic behavior so that it invades and encases neighboring vital structures early.
In most instances by the time the patient becomes symptomatic the disease is inoperable, and the patients usually succumb to the disease within a year of diagnosis.
Approach in the asymptomatic patient
If we are going to play any role in making a difference in this disease, early diagnosis, before involvement of other organs, is a key challenge. Unfortunately finding a small curable carcinoma is a rare occurrence and most the time we are left with a disease that has advanced too far for effective cure. Nevertheless our focus when reviewing the pancreas in anyabdominal CT should be on the head and uncinate process because about 70% of pancreatic carcinomas arise from this part of the pancreas. Since the carcinoma is characteristically hypovascular, we should therefore be looking for a small hypodense rascal in the head of the pancreas. This is not to say of course suggesting that you should not look elsewhere but a focus using probability of finding disease is recommended. You will only find what you look for and so an active mind with a preconceived notion will sometimes yield remarkable results. Our search unfortunately is made more difficult and confounding by a few normal structures that reside in the region, including prominent ducts of the uncinate, and the bile duct itself.
In the following case the subtle nature of pancreatic cancer is noted.
This is a 61 year old male who presented with painless obstructive jaundice and required a stent to relieve the obstruction. On review of the CT scan a subtle hypodense hypovascular mass was noted. Can you see the mass? It is lateral to stent and is just over 1 cms. in diameter. At this stage we are probably too late in our diagnosis for cure. 29970 Courtesy Ashley Davidoff MD
This is a 61 year old male who presented with painless obstructive jaundice and required a stent to relieve the obstruction. On review of the CT scan a subtle hypodense hypovascular mass was noted. In this image the mass is overlaid in maroon. 29970b Courtesy Ashley Davidoff MD
The following case deserves showing to expand on the importance of the analyzing the component parts of the head of the pancreas and the importance of following the pancreatic duct and the bile duct individually to their confluence. Any extra hypodensities must be explained, and heightened sensitivity must be maintained even for the most subtle of changes.
In this CTscan of the abdomen we identify a rounding out of the head and uncinate process with two hypodense components. Associated finding include a dilated gallbladder and a suggestion of intrahepatic bile duct dilatation. Our suspicion on this single image is of pancreatic carcinoma, but how do we interpret the findings in the head? We know that we should have at least two normal hypodensities in this region (bile duct and pancreatic duct), and we also know there is a hypodense mass lurking. The need to review all the images is wanting. 40839 Courtesy Ashley Davidoff MD
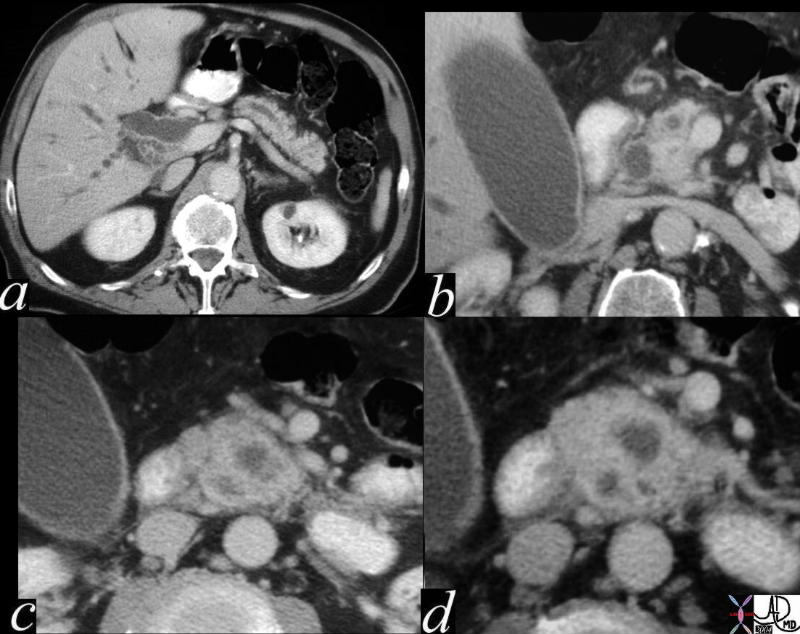
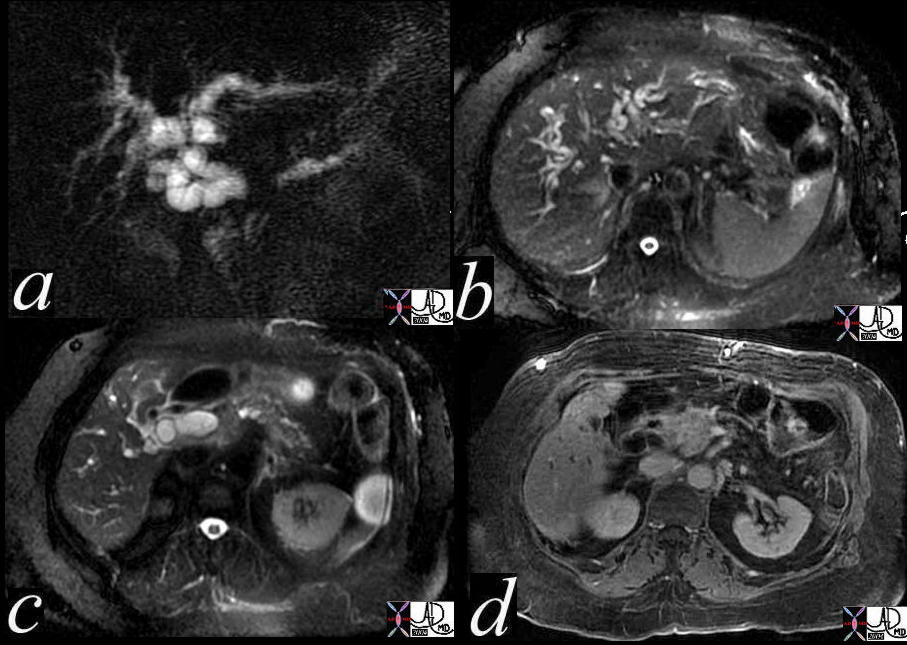
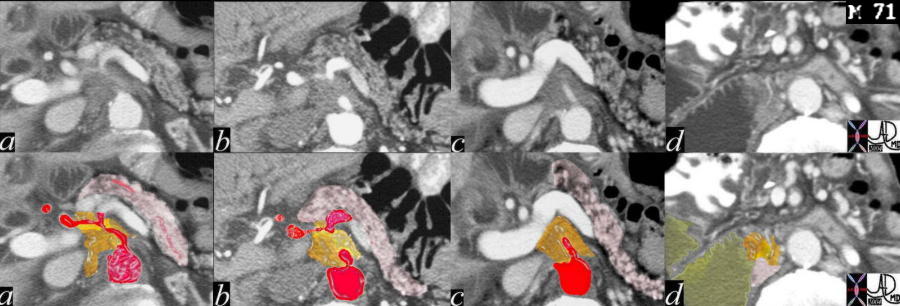
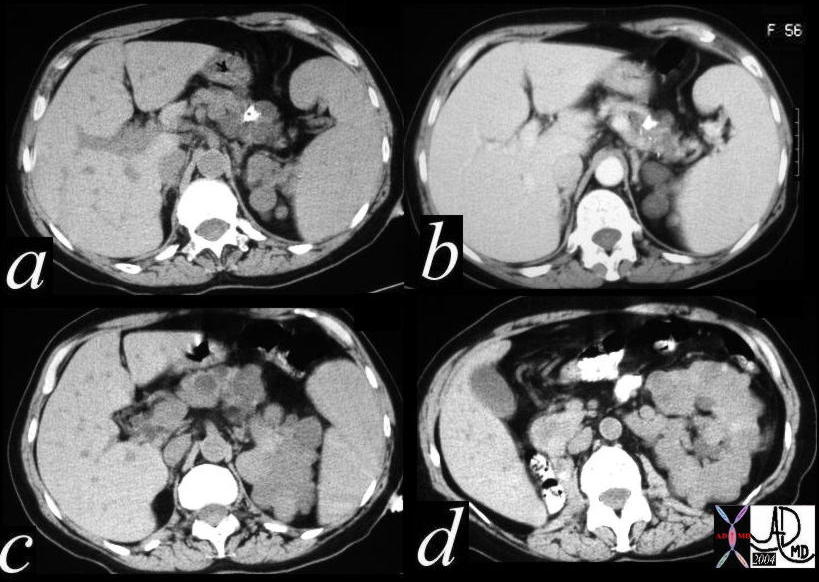
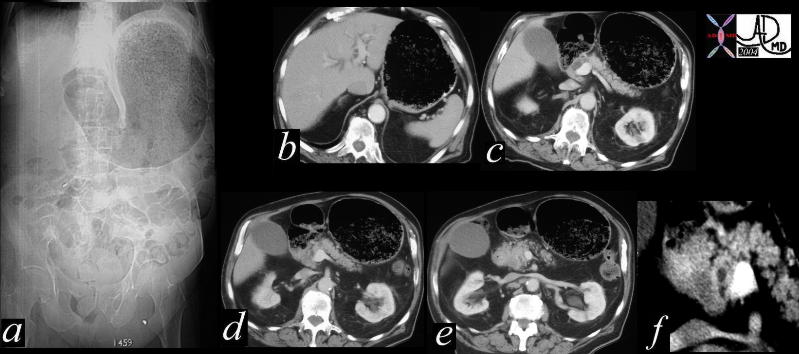
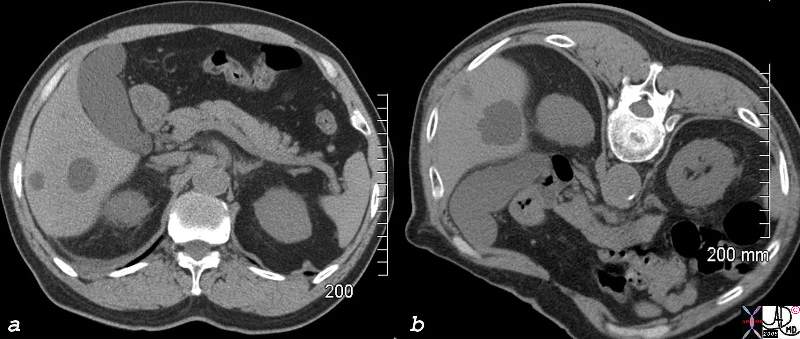
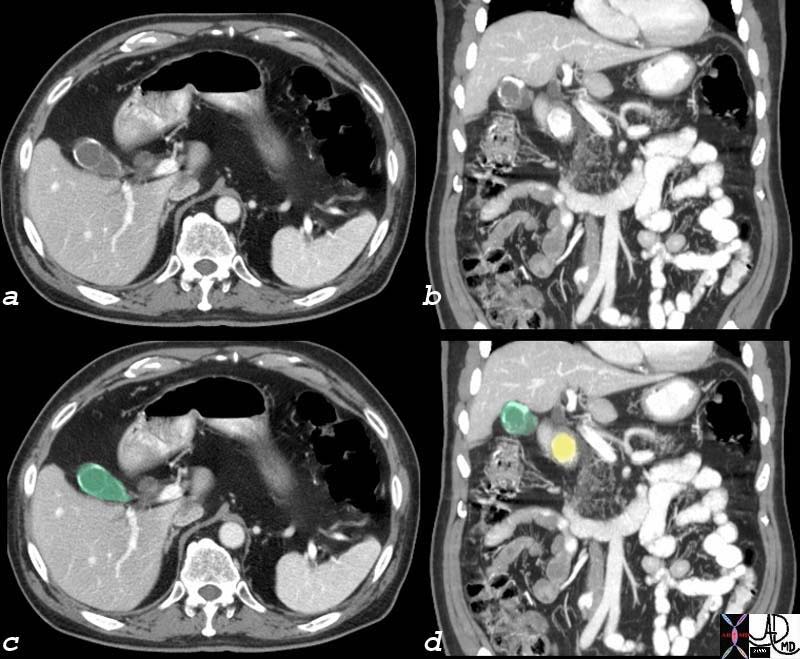
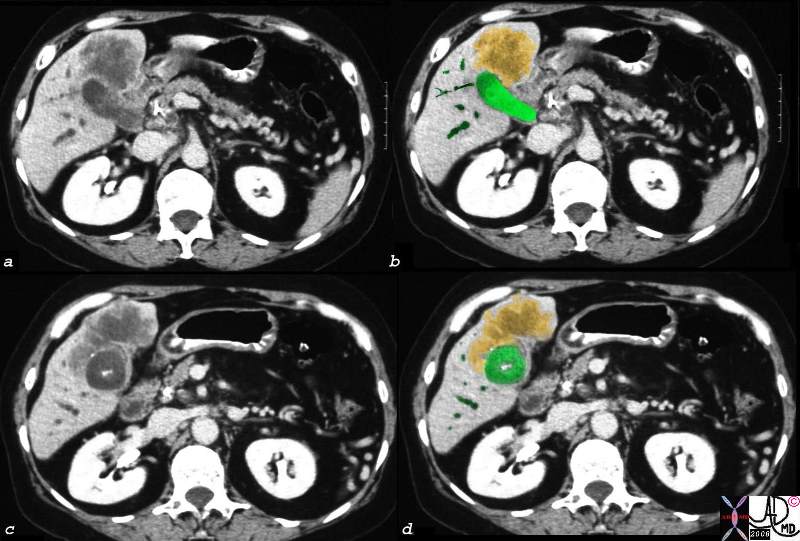
This CT scan series is of a patient with obstructive jaundice and shows a double duct sign suspicious for carcinoma off the head of the pancreas. A dilated pancreatic duct and a dilated CBD (“double duct” sign) is shown (a,b) and then 3 hypodensities and a rotund appearance of the head suggests an extra and unwanted component in the head of the pancreas. Can you identify the unwanted component from these images?. The findings nevertheless are consistent with a primary adenocarcinoma of the pancreas. 40840c01 Courtesy Ashley Davidoff MD
As we review the case with overlays the component parts in the head become clearer. This type of analysis is required in the head with suspicious findings. It is very important to identify pancreatic duct position, bile duct position. Any extra hypodense structures, no matter how small, warrants explanation and or suspicion.
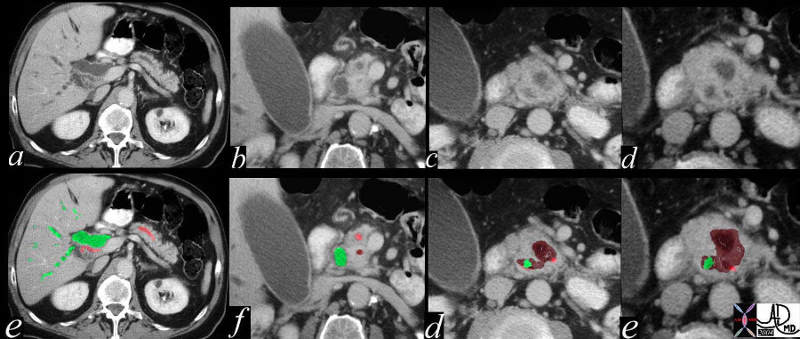
This CT scan series through the pancreas shows the findings of carcinoma of the head of the pancreas in overlay. In a and e the bile duct (green) and pancreatic duct (pink) are both dilated. In “b” and “f” the dilated ducts are approaching each other, and the first hint of a hypodensity (maroon in f) is suggested. In c and g, the bile duct is smaller and the pancreatic duct seems to be pushed to the side by the enlarging mass. The mass, which appears with a matrix of hypodensity and a rim of isodensity starts to enlarge and continues to push and encircle the ducts. (d,h). 40840c02 Courtesy Ashley Davidoff MD
The plea is for careful analysis particularly of the head of the pancreas even on routine abdominal CTscans.
Approach in the symptomatic patient
Approximately 75% of all pancreatic carcinomas occur within the head or neck of the pancreas, 15-20% arises from the body of the pancreas, and 5-10% arises from the tail.
The pancreas has a very central location in the body and has significant and intimate contact or is closely apposed to many organs. The organs are tightly packed in the region of head where the stomach, duodenum, colon, liver, gallbladder, bile duct, right kidney, IVC, SMV, portal vein and SMA lie. The body of the pancreas is related to the stomach which lies anteriorly and the retroperitoneum with nerves aorta and IVC lie posteriorly. The splenic vein lies posteriorly and the splenic artery lies superiorly. The tail nestles in the hilum of the spleen but lies in close contact to the stomach, splenic artery and splenic vein as well.
A reasonable approach to imaging pancreatic carcinoma is to divide the disease into the three parts of the pancreas that it affects, head body and tail, and review the manifestations of the disease in each of these parts.
Nature of the disease.
Pancreatic carcinoma has a scirrhous and scurrilous nature.
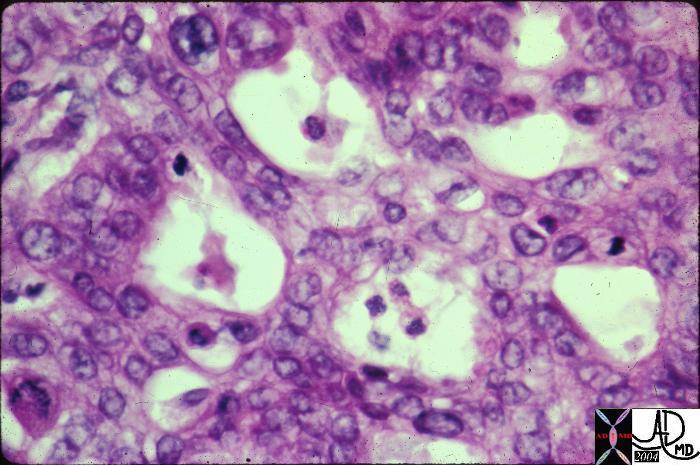
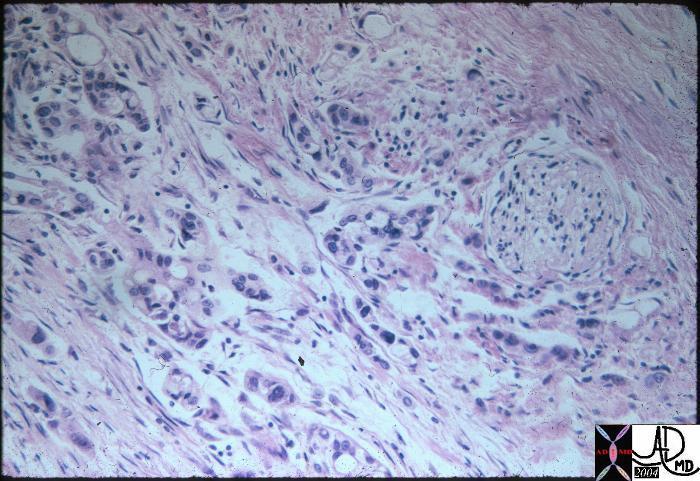
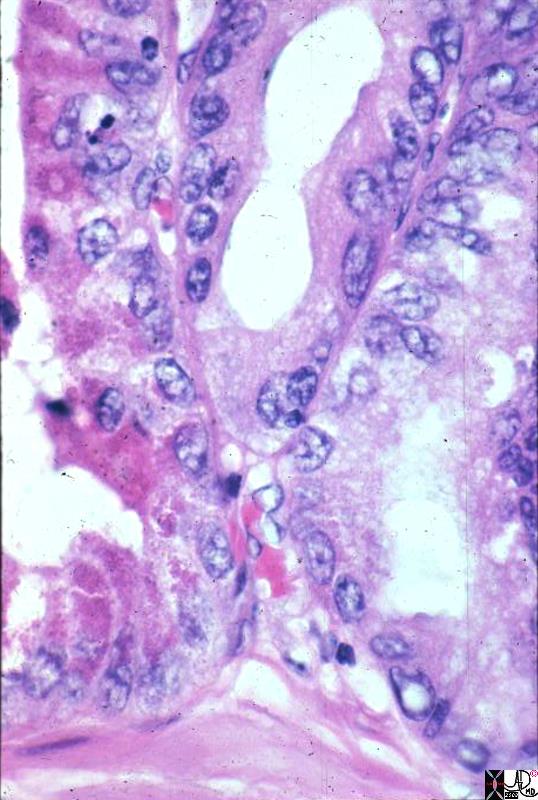
This histopathologic specimen of pancreatic carcinoma shows a heterogeneous pattern to the cells, prominent nuclear to cytoplasmic ratio, and hyperchromatic nuclii. The cells do not obey the rules of the body and are rebels in the community without regard to the body at large. They invade the territory of neighboring structures. 15311 Courtesy Barbara Banner MD
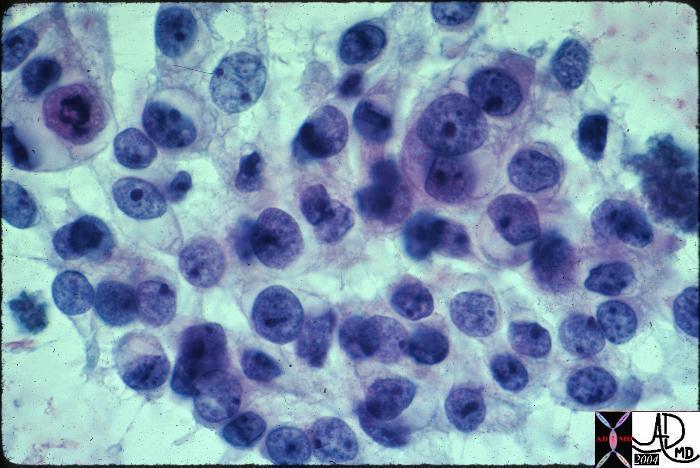
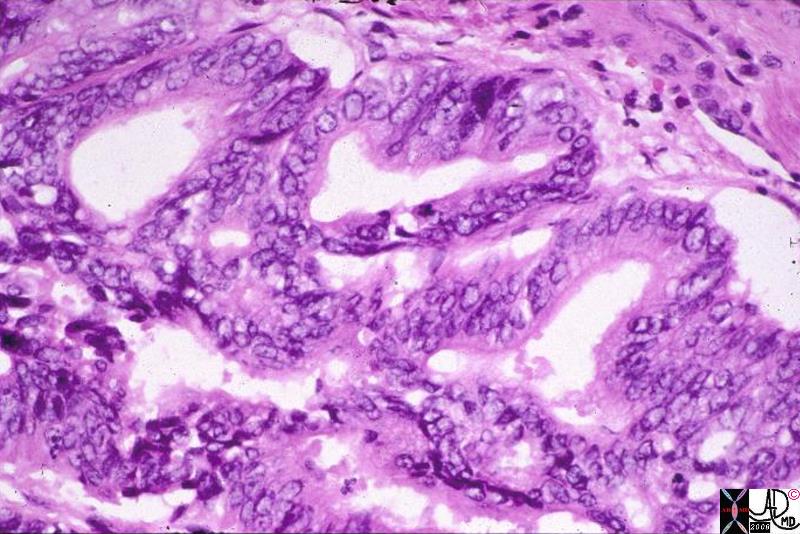
The cells of adenocarcinoma of the pancreas are well appreciated in this cytological specimen from a biopsy. Noted is the heterogeneous pattern to the cells, prominent nuclear to cytoplasmic ratio, and hyperchromatic nuclii. 15310 Courtesy Barbara Banner MD
Thus the aggressive nature of malignant cells of the pancreas is characteristic of all malignant tissue. In addition to their aggressive nature they are characterized by desmoplastic behavior. As a result they encircle, constrict and strangle their neighbors.

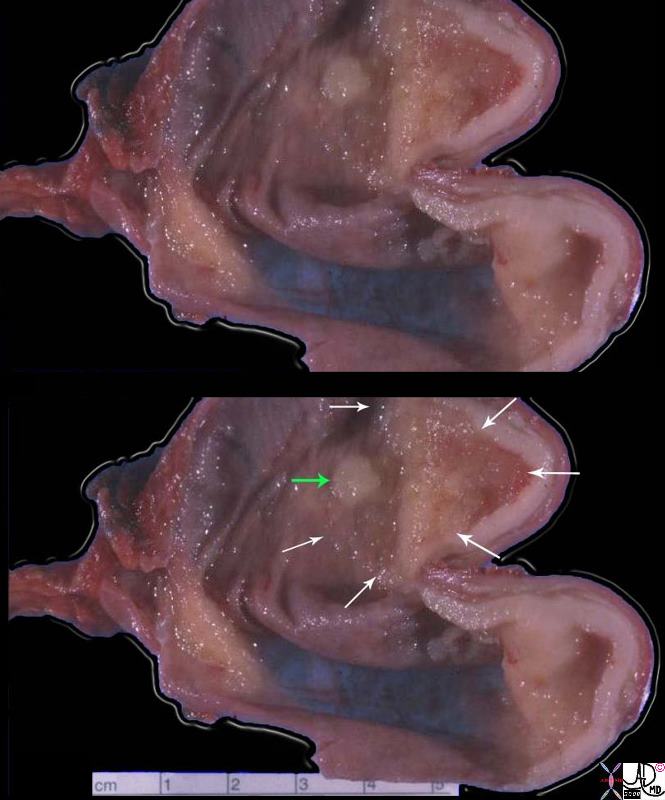
The grosspathology specimen shows a white mass in the middle of the image. It was extremely hard to the touch because of the fibrosis shown at histopathology. The desmoplastic or fibrous nature of the tumor leads to encasement and narrowing of contiguous structures. This fibroblastic nature of the disease is characteristic of adenocarcinoma of the pancreas. 15307 Courtesy Barbara Banner MD
Aggression and desmoplasia are thus the pathological hallmarks of adenocarcinoma of the pancreas. Hypovacsularity is the radiologic hallmark
Head.
Ducts
The desmoplastic nature of the disease affects in characteristic location being near or within a few centimeters of the ampulla.
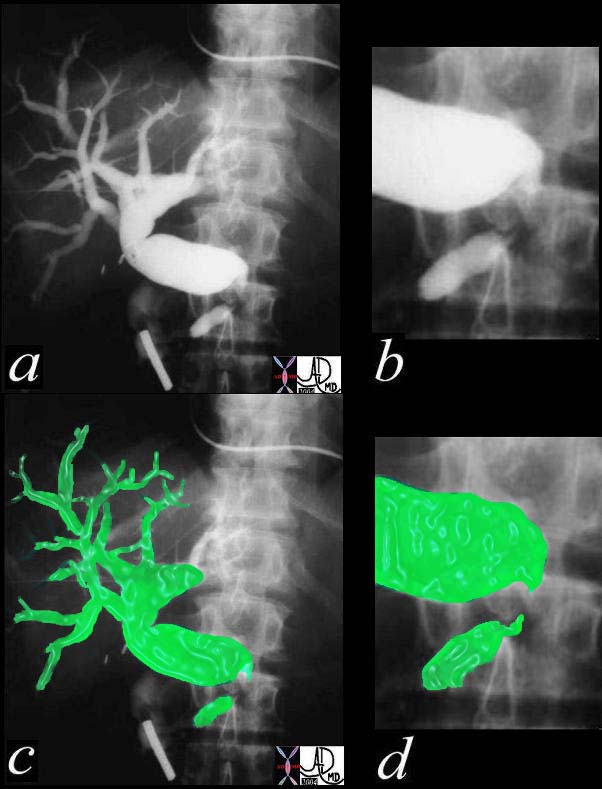
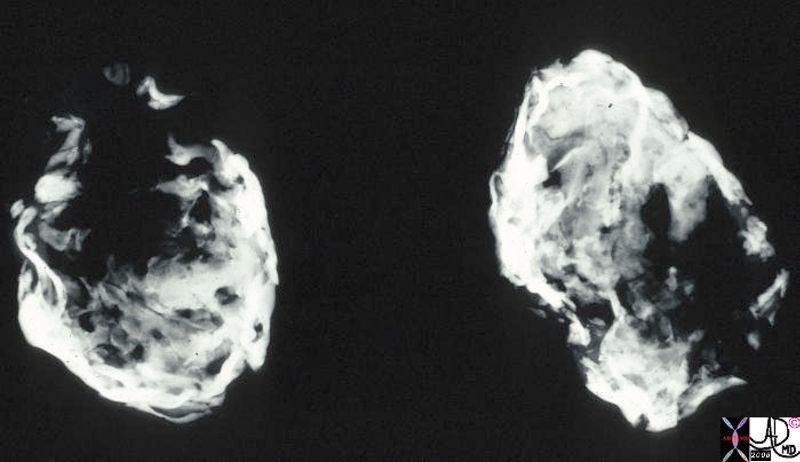
The following images come from a percutaneous transhepatic cholangiogram 9PTCA) and show a concentric stricture around the distal common bile duct with rat tailing of the stricture and secondary upstream dilatation. The location is characteristic, but not necessarily pathognomonic for carcinoma of the head of the pancreas. 04835c03 Courtesy Ashley Davidoff MD
The head of the pancreas houses the common bile duct which delivers 600-700ccs of bile to the duodenum per day. The pancreatic duct and bile duct fuse in the ampulla just prior to their common entrance into the duodenum. The bile duct is one of the closest allies if not the closest buddy of the pancreatic duct. In fact they are bosom buddies even from the time of organogenesis. On the other hand although they were born together and function together in health, in the presence of pancreatic carcinoma in the head they will commonly get sick together as well (“ ‘til death do us part”). The double duct sign implies the enlargement of both the bile duct and pancreatic duct and is almost pathgnomonic of carcinoma of the head of the pancreas. The association is taken one step further when as a result of the obstruction the gallbladder gets affected. This is part of the Courvoisier’s law that states ‘if in the presence of jaundice the gallbladder is palpable, then the jaundice is unlikely to be due to a stone.’ As an extension of this law, if in addition the jaundice is painless then carcinoma of the head of the pancreas is likely.
The case below demonstrates a classical double duct sign.
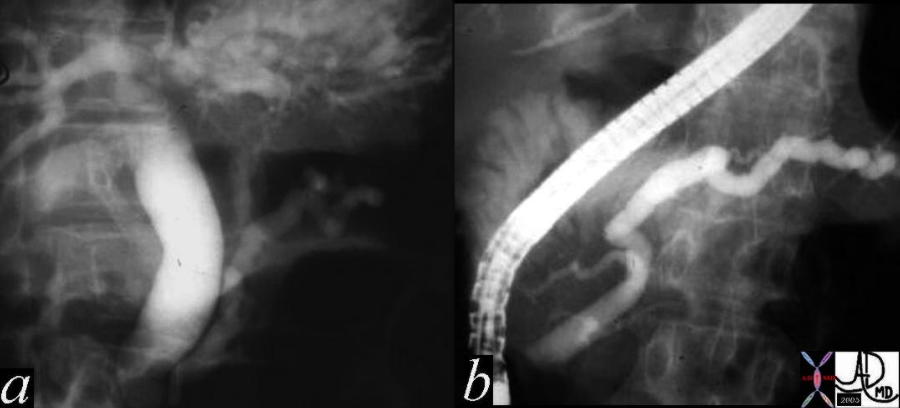
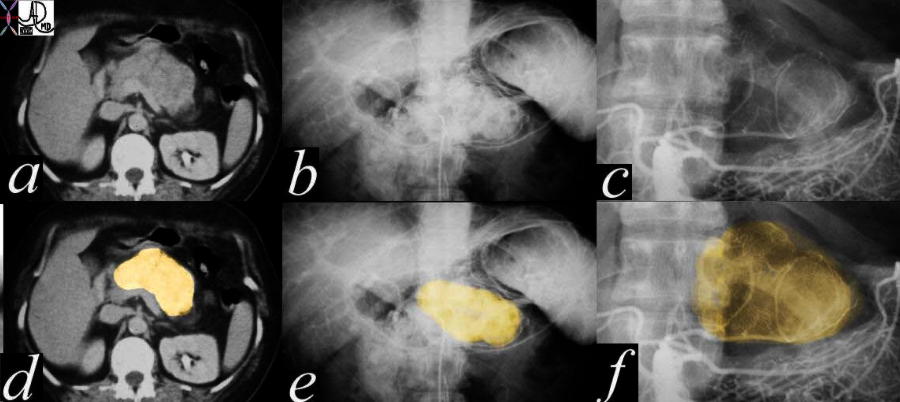
A 57 year old female presents with jaundice. Her ERCP shows dilatation of the bile duct and pancreatic duct – the “double duct” sign characteristic of adenocarcinoma of the head of the pancreas. In this case the stricture appears quite distal. Chronic pancreatitis can also rarely cause the “double duct” sign. In this case an ampullary carcinoma was the cause explaining the distal position of the strictures. 04655c03 Courtesy Ashley Davidoff MD
The combination of images below reflects the changes of the above case using a multimodality approach with pathological proof.
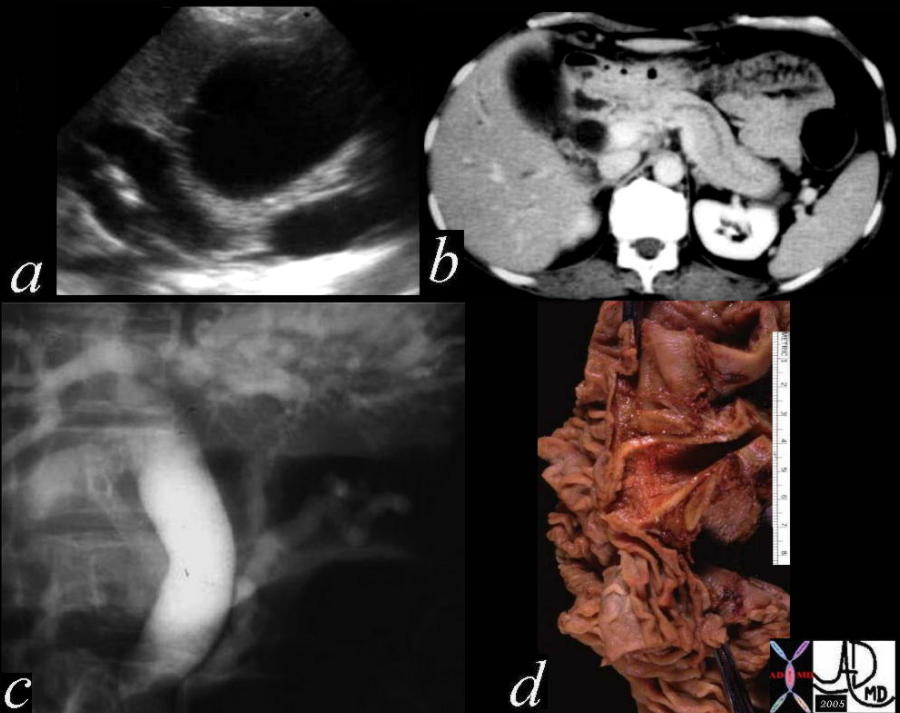
This is a series of images from the case history of a 57 year old female who presented with jaundice. The US image (a) shows a dilated bile duct and dilated pancreatic duct with no large mass between them. The CT shows a les impressive, but prominent pancreatic duct. The ERCP suggests a “double duct” sign. The pathology confirmed an ampullary carcinoma. 04655c05 Courtesy Ashley Davidoff MD
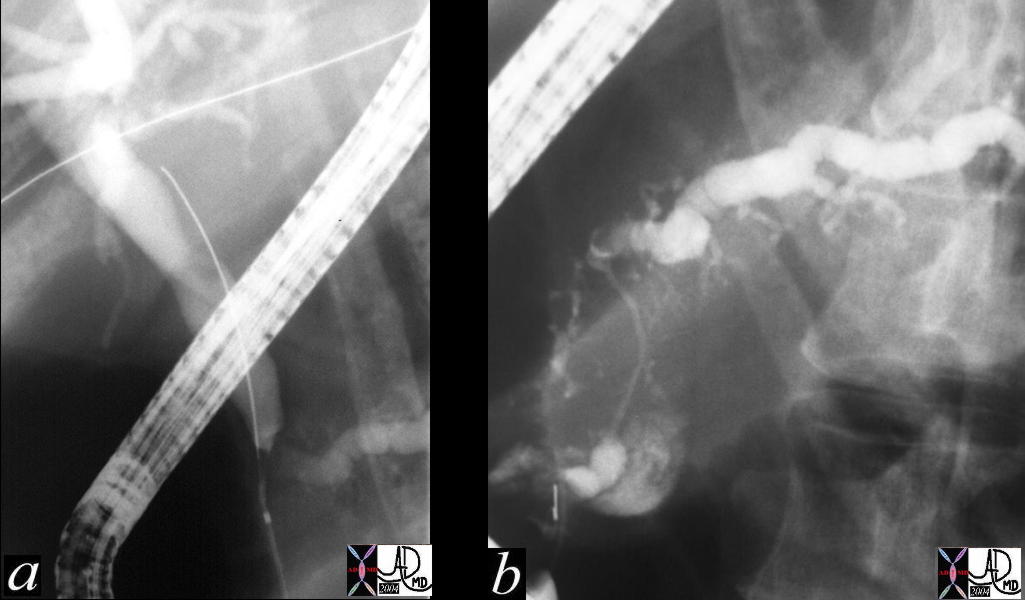
This ERCP shows a double duct sign with a dilated CBD and pancreatic duct. These findings are consistent with a primary adenocarcinoma of the pancreas. Chronic pancreatitis is a remote possibility. 31062c01 Courtesy Ashley Davidoff MD
Double duct sign is also used in other modalities and has the same implications.
This CT scan through the pancreas shows a dilated pancreatic duct and a dilated CBD (“double duct” sign). These findings are consistent with a primary adenocarcinoma of the pancreas. Chronic pancreatitis is a remote possibility. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. 40837 Courtesy Ashley Davidoff MD
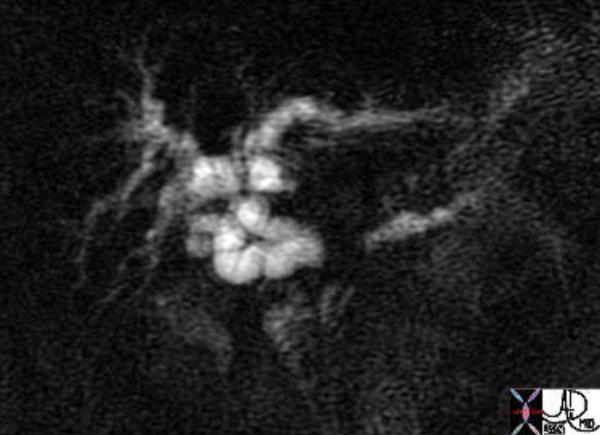 The image from an MRCP shows the MRI version of the double duct. The separation of the two ducts suggests a large size of the mass. This patient had pancreatic carcinoma. 41371 Courtesy of Ashley Davidoff MD
The image from an MRCP shows the MRI version of the double duct. The separation of the two ducts suggests a large size of the mass. This patient had pancreatic carcinoma. 41371 Courtesy of Ashley Davidoff MD
The combination of images below reflects the changes of the above case at different levels. Cranially the liver is seen and caudally the pancreas is seen.
The image from an MRCP shows the MRI version of the “double duct” sign. The separation of the two ducts suggests a large size of the mass (a). Image b shows intrahepatic biliary dilatation, while image c shows CBD dilatation. Image d shows a mass in the head of the pancreas on the contrast enhanced sequence. This patient had pancreatic carcinoma. 41371c Courtesy of Ashley Davidoff MD
There are instances where the double duct sign represents other diseases.
This is an ERCP showing a “double duct” sign. With the heavy intraductal calcification chronic alcoholic pancreatitis is definite. It is conceivable that the patient has a superimposed malignancy. In this case the double duct was caused by the strictures of the ducts caused by chronic pancreatitis. 41245c06 Courtesy Ashley Davidoff MD
At first glance this image from an ERCP looks like a double duct sign. In fact it does show that both ducts are dilated, but for different reasons other than cancer. The main pancreatic duct drains into the accessory duct of Santorini, while the CBD drains in usual fashion into the ampulla. This is a case of pancreas divisum. No pancreatic cancer was found on further workup. The etiology of the mild dilation is probably due to benign narrowing of both ducts at their insertion sites. 40615 Courtesy Ashley Davidoff MD
Arteries and Veins in the head
The gastroduodenal artery is closely linked to the head of the pancreas, and the branches of the pancreaticoduodenal arcade lie within the head of the pancreas. In years prior to the exquisite detail provided by CT and MRI, an angiogram was part of the workup of patients with suspected carcinoma of the pancreas for both confirmation of the diagnosis but also for operability. The presence of encasement of the vessel supported the diagnosis, and the presence of portal vein encasement specifically suggested inoperability. The following cases exemplify the discussion.
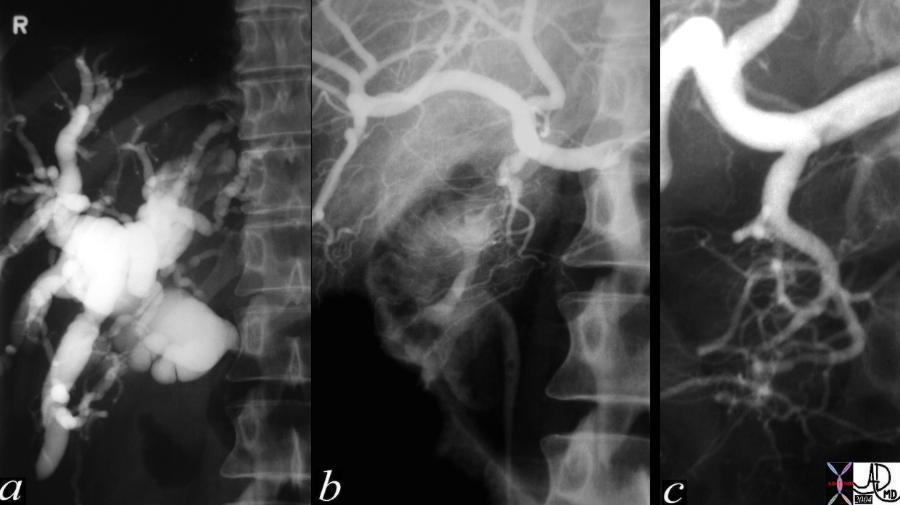
This series of percutaneous transhepatic cholangiography, PTCA (a), and arteriography (b) magnified in c, reveal an obstructed and dilated intrahepatic biliary system and encasement of some of the branches of the pancreaticoduodenal arcade.40328c Courtesy Ashley Davidoff MD
The following images are from the same case and the portal venous phase is demonstrated.
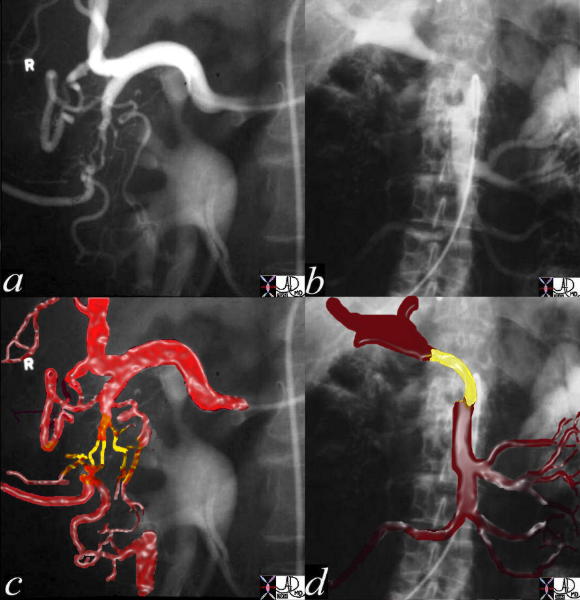
This series of arteriography of the common hepatic artery (a,c), with portal venous phase from an SMA injection(b,d) reveals the encasement of the pancreaticoduodenal arteries (c, yellow) magnified and portal vein (d yellow) The location and characteristic encasement point to pancreatic adenocarcinoma of the head of the pancreas. The portal vein involvement suggests inoperability. Courtesy Ashley Davidoff MD
The advent of MDCT has brought better resolution of soft tissue changes. The finding of a necklace of tumor around the SMA, and the degree to which it surrounds the SMA is being used as a predictor of operability.
This CT scan through the pancreas shows a small mass in the uncinate process of the pancreas associated with total encasement of the celiac axis. The CBD is dilated. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. Based on the desmoplastic nature of the process the tumor is most likely an adenocarcinoma. 20599 Courtesy Ashley Davidoff MD
This CT scan through the pancreas is a series with overlay from the above case, and shows a small mass in the uncinate process of the pancreas associated with encasement of the celiac axis and SMA, with a dilated CBD. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. Based on the desmoplastic nature of the process, the tumor is most likely an adenocarcinoma. The artery is in red the tumor orange and the normal pancreas is pink. 20607c06 Courtesy Ashley Davidoff MD
Stomach
40851c Courtesy Ashley Davidoff MD code abdomen stomach distended code stomach fx bezoar code pancreas pancreatic lateral uncinate process fx mass code dx carcinoma of the uncinate pancreas complicated by gastric outlet obstruction imaging radiology plain film KUB CT scan code neoplasm malignant primary tumor cancer mechanical code medical students 5 star
Duodenum
The head of the pancreas is housed in the c sweep of the duodenum and encasement at any point in the “c “ can be affected.
This CT scan through the pancreas shows a small mass in the uncinate process of the pancreas associated with a dilated and obstructed duodenum. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. Based on the desmoplastic nature of the process the tumor is most likely an adenocarcinoma. 20601 Courtesy Ashley Davidoff MD
This CT scan through the pancreas shows a hypodense mass in the pancreatic head, associated with a central dystrophic calcification and a dilated pancreatic duct. These findings are consistent with a cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the dilated duct. The calcifications in the spleen are granulomatous in origin. 19394c01 Courtesy Ashley Davidoff MD
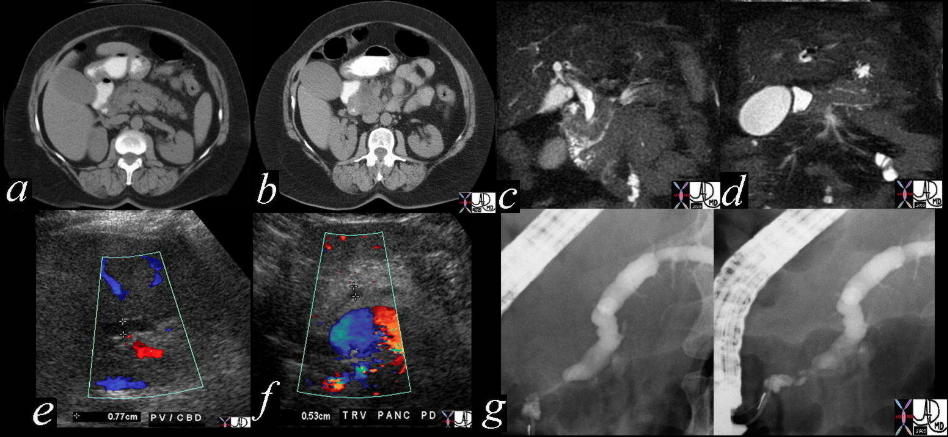
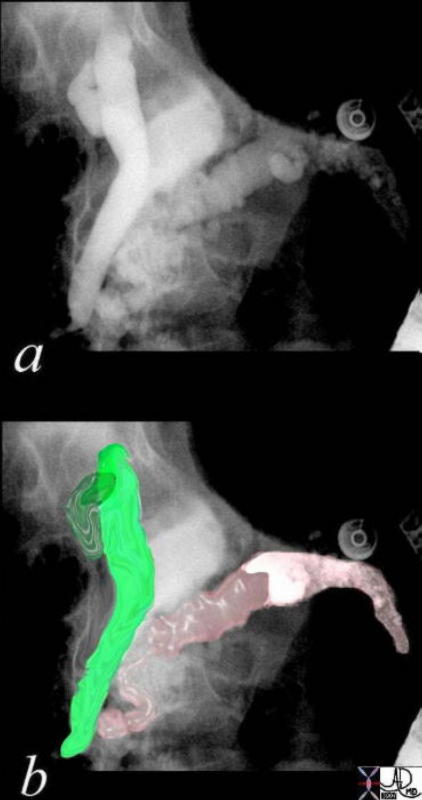
The CT scan, MRI, US and ERCP of the pancreas shows a dilated pancreatic duct and a dilated CBD (“double duct” sign). These findings are consistent with a primary adenocarcinoma of the pancreas. 41293a16c Courtesy Ashley Davidoff MD
Body
The central part of the pancreas is closest to the vessels nerves lymphatics of the abdomen. Pancreatic adenocarcinoma shows an affinity for nerves and the involvement of the nerve results in significant back pain in patients with pancreatic carcinoma. This is more common with body and tail carcinomas.
The body and tail of the pancreas are close to the lymphatics and nerves. In this histological section the rounded nerve seen to the right in the image is surrounded by advancing malignant pancreatic carcinoma seen as cluster of blue nuclii.
Courtesy Barbara Banner MD
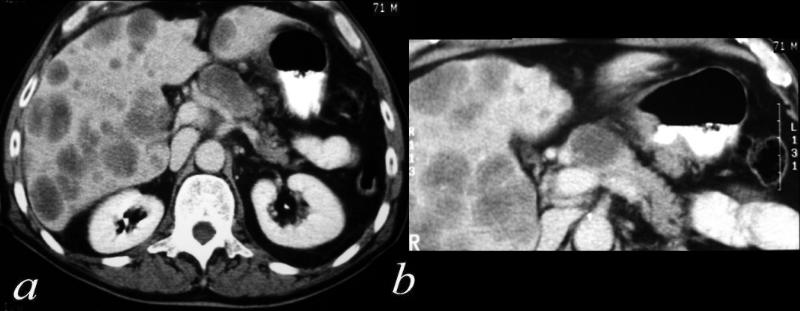
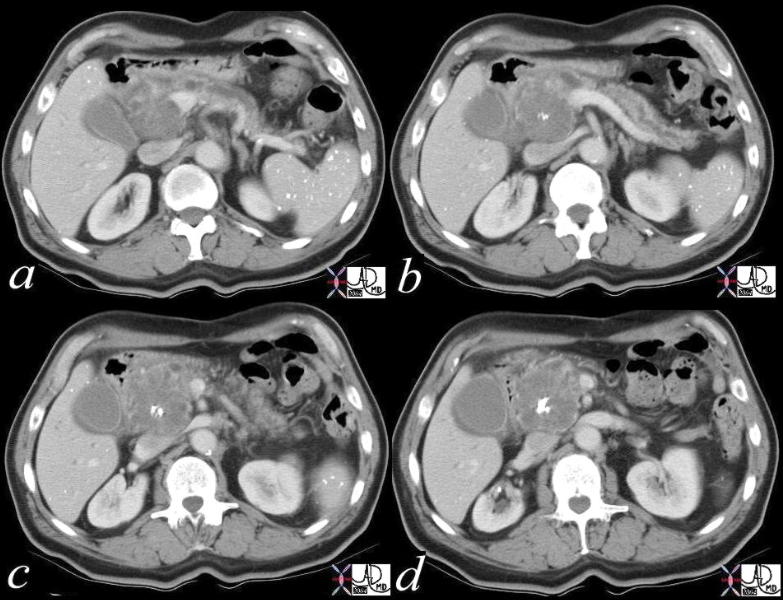
The CT scan of the abdomen of a 71 year old male shows a hypovascular mass in the body of the pancreas with widespread metastatic disease in the liver. Some of the lesions in the liver are larger than the primary tumor. 40343c Courtesy Ashley Davidoff MD
Duct in the body
In patients with obstructed ducts there is usually secondary

This CT scan through the pancreas shows a mass in the neck and body of the pancreas associated with pancreatic duct dilatation and secondary atrophy in the pancreatic tail. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. Based on the desmoplastic nature of the process the tumor is most likely an adenocarcinoma. 30101a05 Courtesy Ashley Davidoff MD
Arteries and Veins
This CT scan through the pancreas shows a mass in the body of the pancreas associated with encasement of the portal vein and splenic artery (subtotal occlusion) with an almost complete encirclement of the celiac axis by a necklace of aggressive tissue. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas. Based on the desmoplastic nature of the process the tumor is most likely an adenocarcinoma. Courtesy Ashley Davidoff MD18103
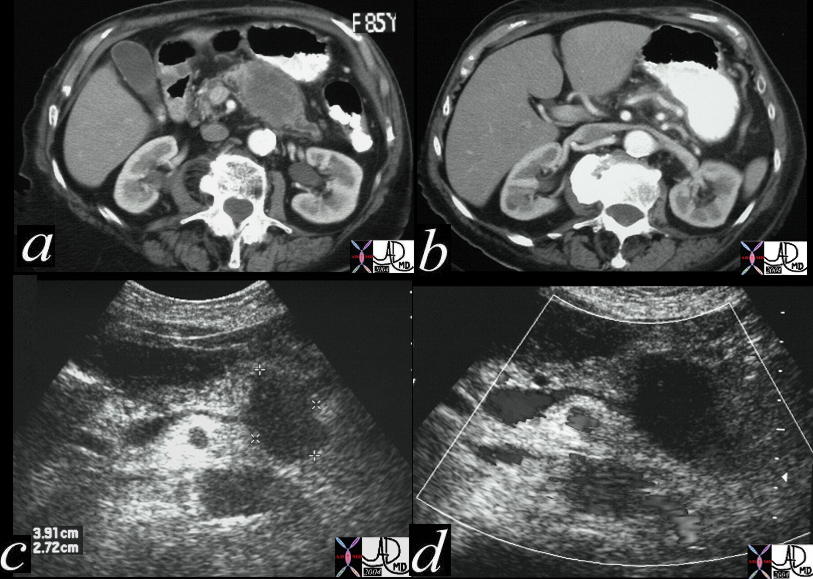
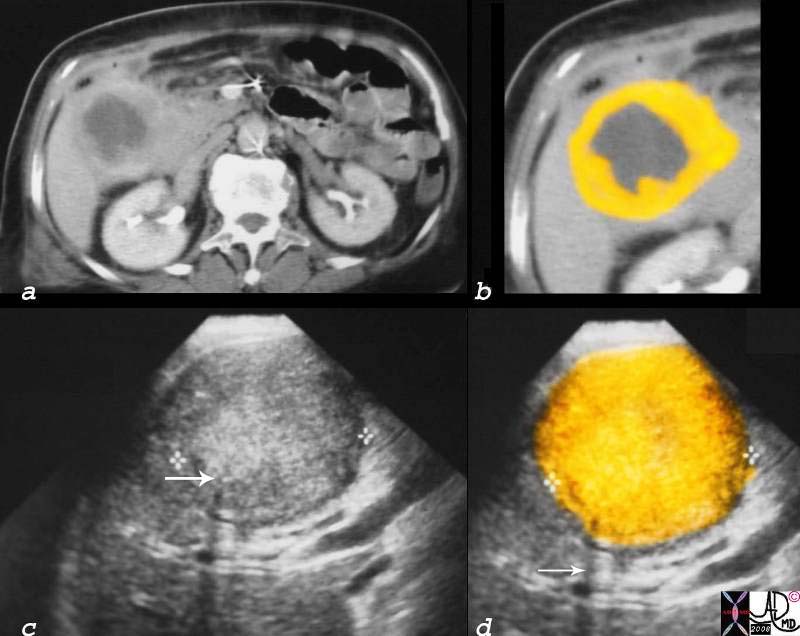
The CT scan of the abdomen of a 85 year old female shows a hypovascular mass in the body and tail of the pancreas (a) which has resulted in splenic vein compromise and the development a large venous collateral seen coursing over the greater curvature of the stomach. The mass is hypoechoic (c) and hypovascular d) on the US. 24942c Courtesy Ashley Davidoff MD
Unusual masses

This CT scan through the pancreas shows a mass in the body of the pancreas associated with metastatic liver disease. The patient presented with Cushingoid features which was associated with ectopic ACTH biochemistry. An adrenal nodule is noted reflective of hyperplasia from the effect of ACTH. The mass at autopsy was consistent with a malignant gastrinoma associated with ectopic ACTH production. Courtesy Ashley Davidoff MD 19859
This is a series of images from a middle aged female with a hypervascular mass in the body of the pancreas. Since adenocarcinoma of the pancreas tends to be hypovascular it is unlikely that the histological type is the common form. In this case the diagnosis was a micronodular carcinoma 40640c02 Courtesy Ashley Davidoff MD ..
This CT scan through the pancreas shows a complex cystic mass with central calcification in the tail of the pancreas associated with complex masses in the left kidney and surgically absent right kidney. These findings are consistent with a diagnosis of von Hippel-Lindau syndrome with a variety of cystic and solid, benign and malignant tumors of the pancreas and kidney. 40463c Courtesy Ashley Davidoff MD
Tail
Spleen
This CT scan through the pancreas shows a mass in the tail of the pancreas associated with splenic invasion ascites, a probably liver metastasis, and thickened omentum. These findings are consistent with a diagnosis of a primary carcinoma of the pancreas, with metastatic disease. 20796 Courtesy Ashley Davidoff MD
Peritoneum
Sometimes more than 2/3 of the circumference of the tail of the pancreas is covered by peritoneum making it a peritoneal structure. Thus more than any of the other parts of the pancreas malignancy in the tail may spread directly into the peritoneal cavity.
This CT scan through the pancreas shows a cystic mass in the pancreatic tail associated with thickened gastrolienal ligament and ascites. This case represents transperitoneal spread of a known pancreatic carcinoma. Metastatic nodules are also noted in the liver. 20114 Courtesy Ashley Davidoff MD
Cystadenocarcinoma
The cystic lesions of the pancreas are discussed as a separate entity in detail. However they are a variant of carcinoma but have a different biology and nature. Specifically they do not demonstrate the desmoplastic behavior of the more commonly occurring scirrhous adenocarcinoma.
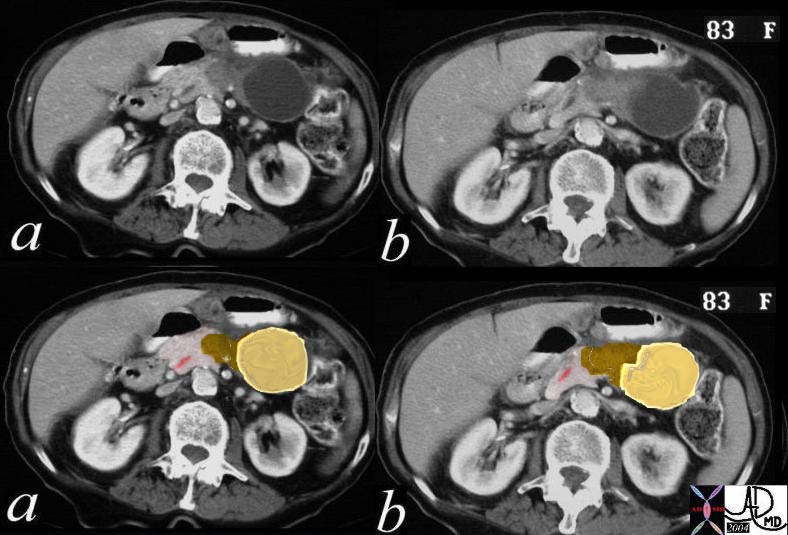
This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass in the tail with a more solid appearing tail that is in the body. (a,b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
References
Courvoisier LJ. Casuistisch-statistische beitrage zur pathologie und chirurgie der gallenweger. Leipzig: Vogel; 1890.
Pancreatic Carcinoma from Radiologyassistant.nl web pressentation






 Carcinoma Thickening and Granular Appearance
Carcinoma Thickening and Granular Appearance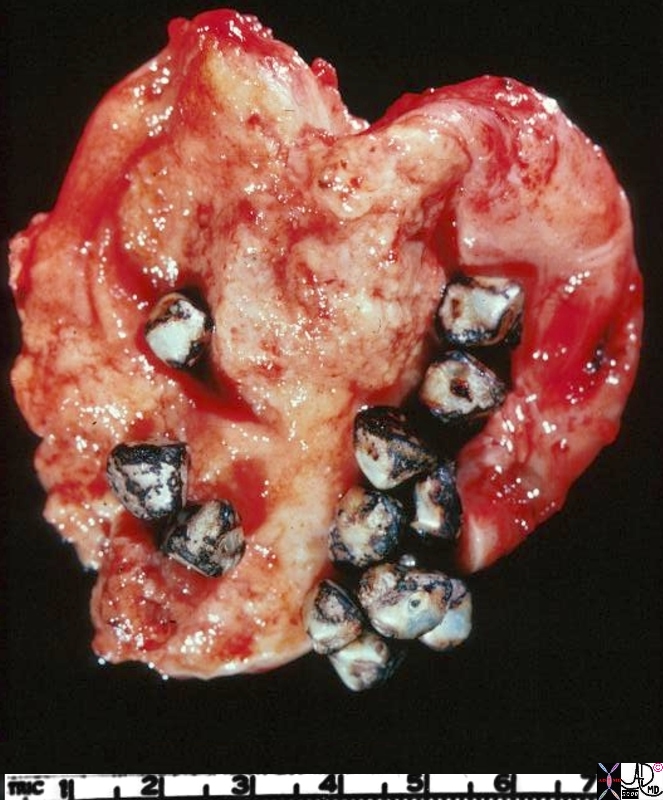 Carcinoma – Mass
Carcinoma – Mass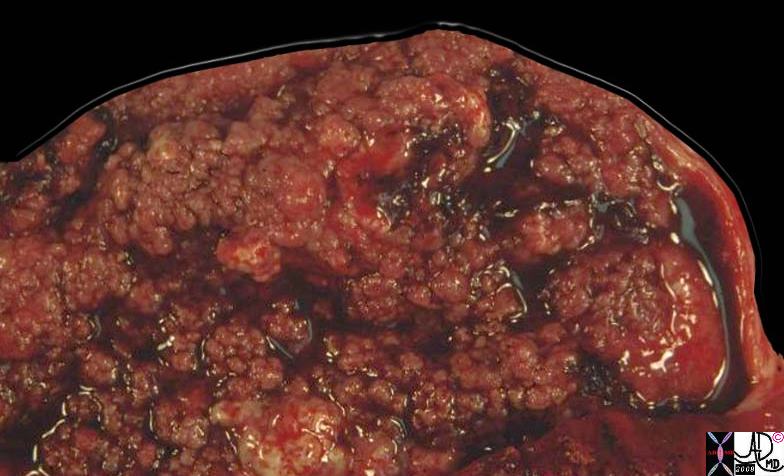



 Carcinoma – Back to Back Gland Arrangement
Carcinoma – Back to Back Gland Arrangement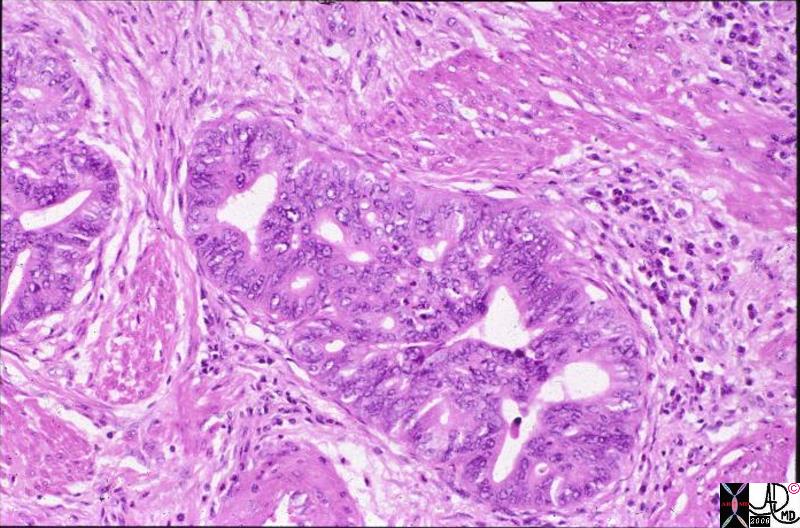 Carcinoma – Back to Back Gland Arrangement and Irregular Nuclii
Carcinoma – Back to Back Gland Arrangement and Irregular Nuclii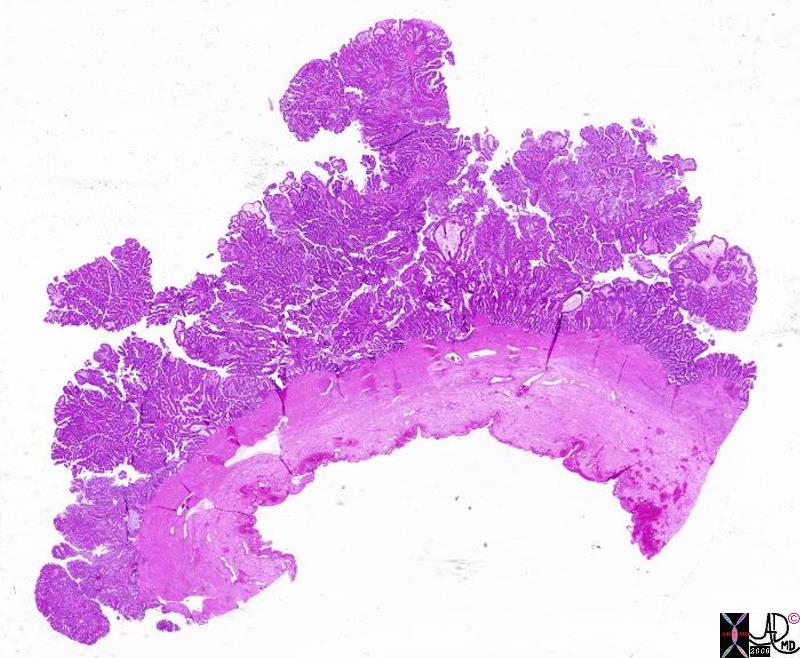 Carcinoma – Papillary Form
Carcinoma – Papillary Form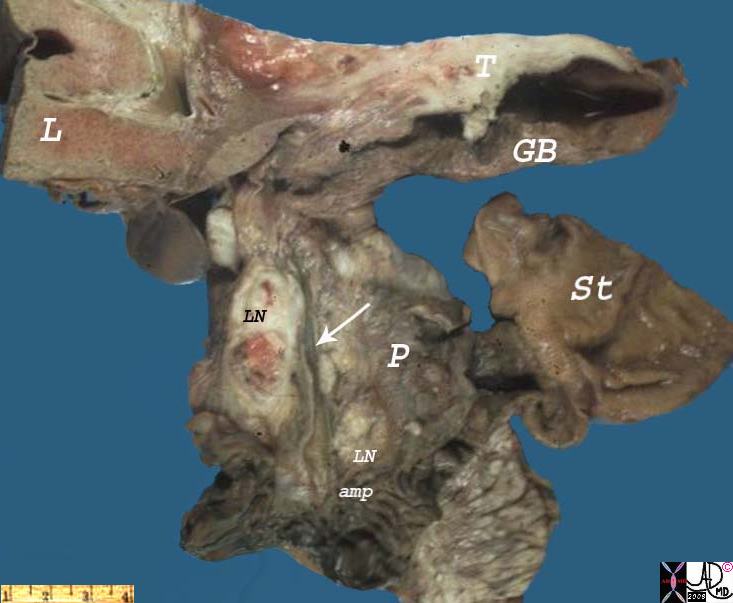 Carcinoma – Lymph Nodes
Carcinoma – Lymph Nodes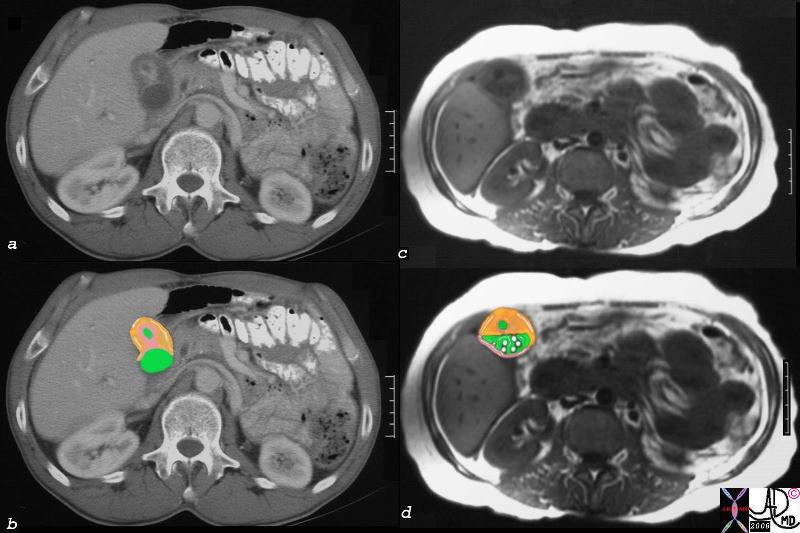 Carcinoma of the Fundus CT and MRI
Carcinoma of the Fundus CT and MRI
 Direct Invasion into the Liver and Bile Duct Obstruction
Direct Invasion into the Liver and Bile Duct Obstruction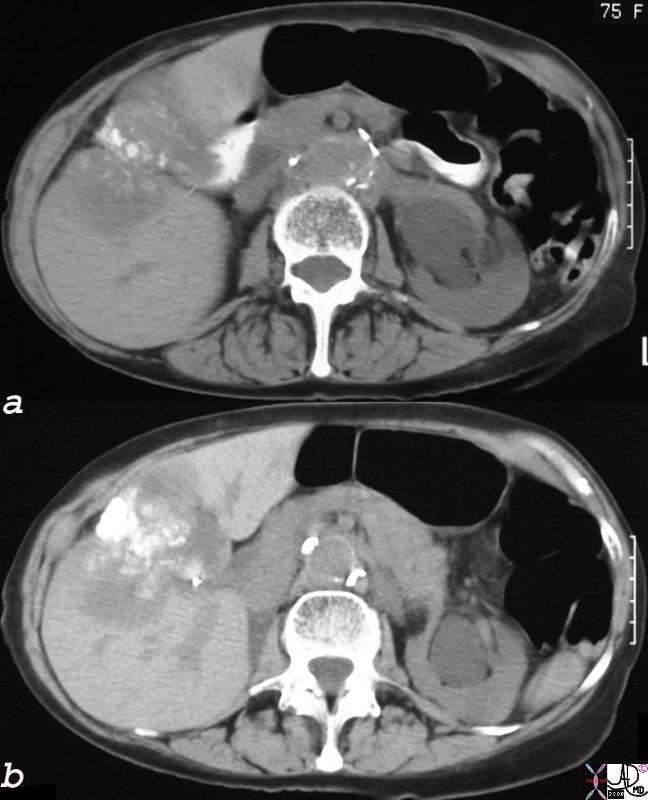 Dystrophic Calcification – Carcinoma of the Gallbladder Extending into the Gallbladder Fossa
Dystrophic Calcification – Carcinoma of the Gallbladder Extending into the Gallbladder Fossa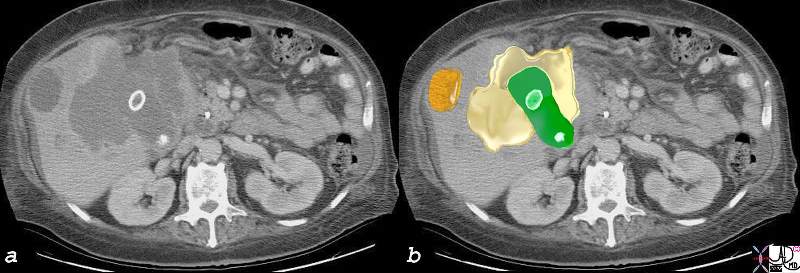 Local Invasion and Separate Liver Mestastasis
Local Invasion and Separate Liver Mestastasis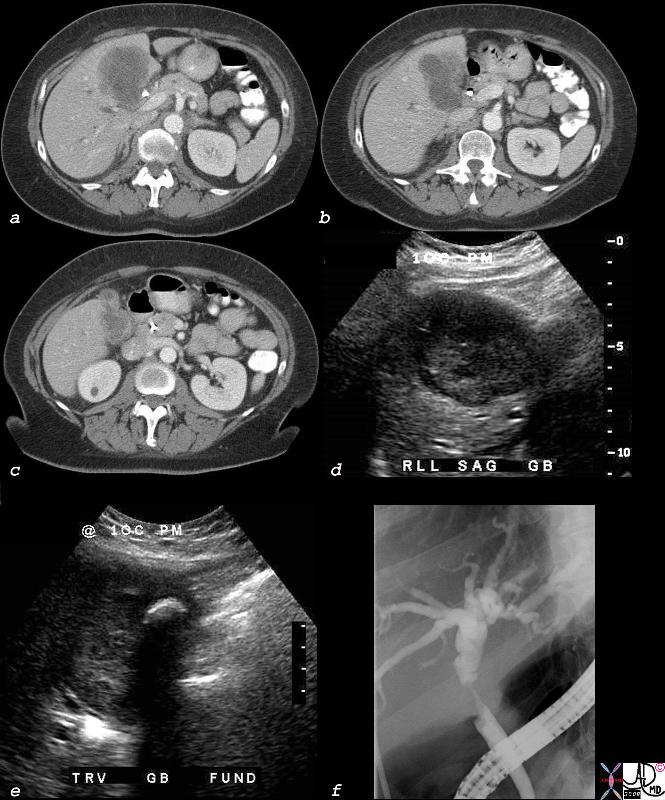
 Luminal Invasion
Luminal Invasion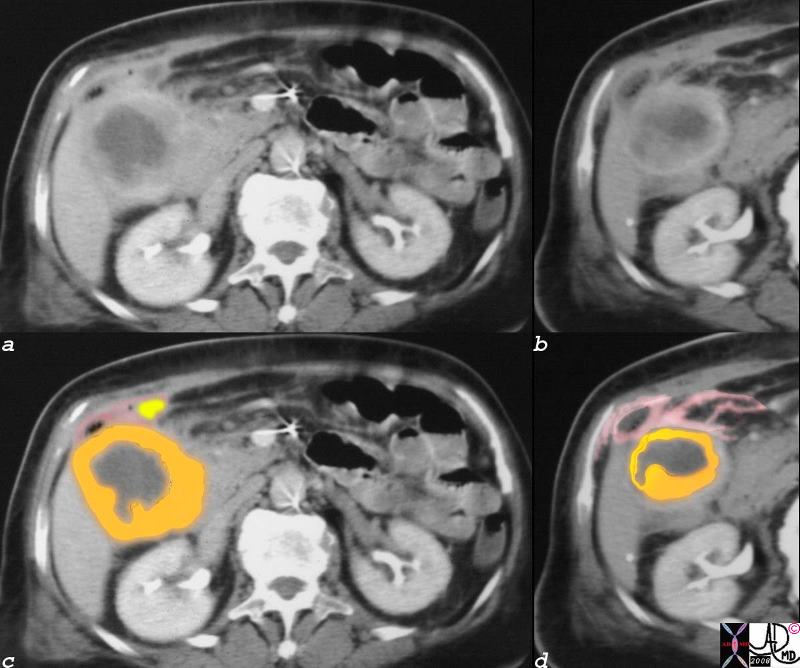 Gallbladder Carcinoma with Perforation and Abscess Formation
Gallbladder Carcinoma with Perforation and Abscess Formation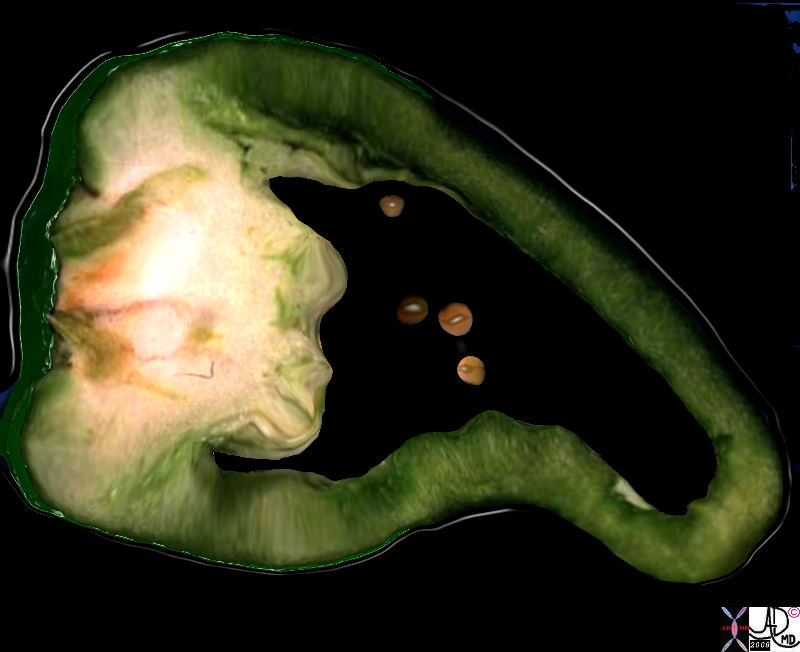

 Ulcerating Squamous Cell Carcinoma of the Esophagus
Ulcerating Squamous Cell Carcinoma of the Esophagus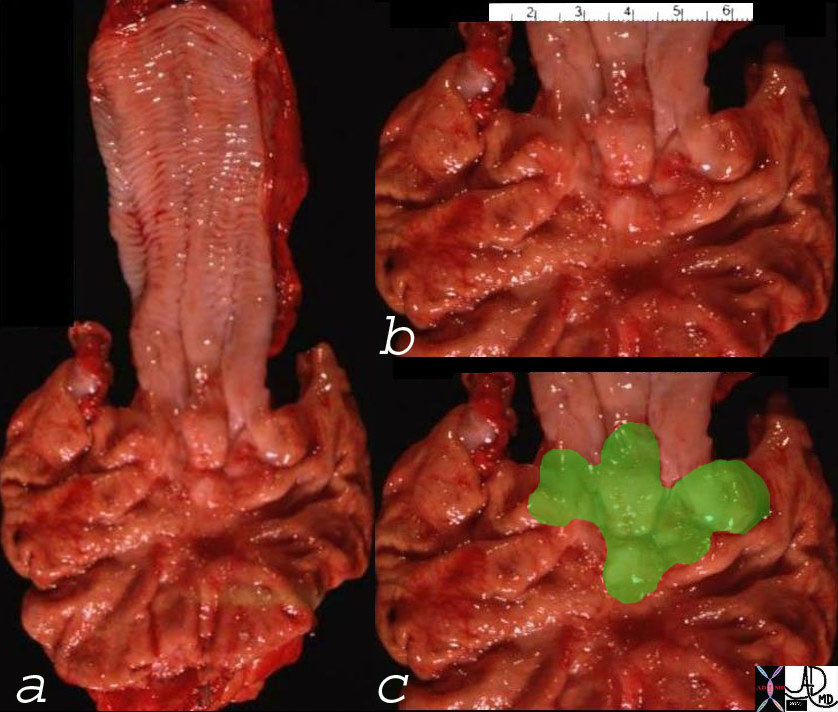 Ill Defined GE Junction Tumor – Adenocarcinoma
Ill Defined GE Junction Tumor – Adenocarcinoma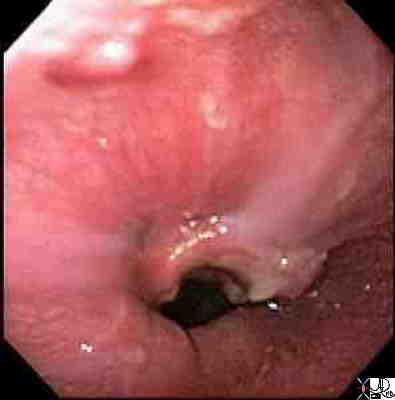 Carcinoma of the Esophagus
Carcinoma of the Esophagus Carcinoma of the Esophagus
Carcinoma of the Esophagus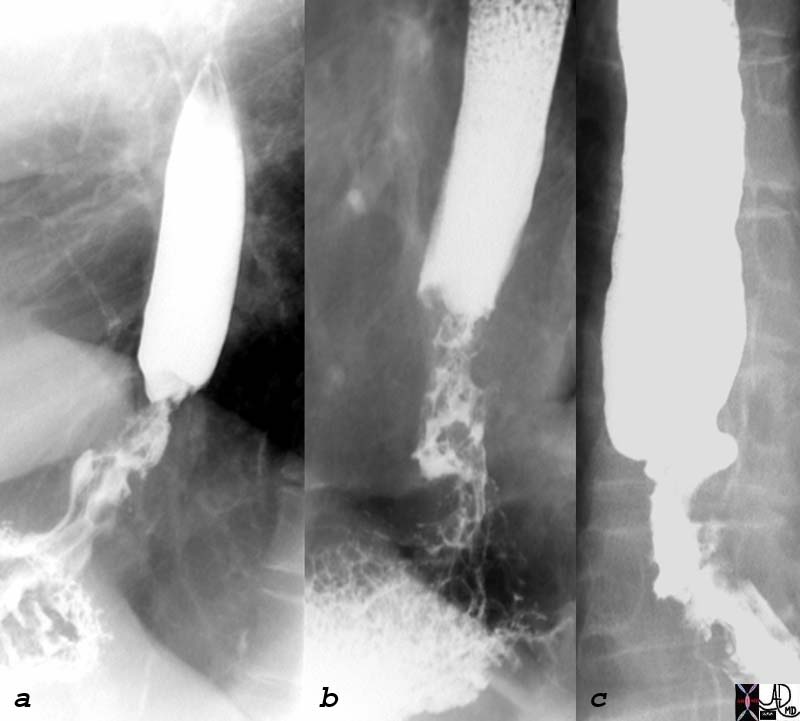 Irregular Distal Esophagus with Stricture – Adenocarcinoma of the GE junction
Irregular Distal Esophagus with Stricture – Adenocarcinoma of the GE junction Long Relatively Smooth Malignant Stricture
Long Relatively Smooth Malignant Stricture
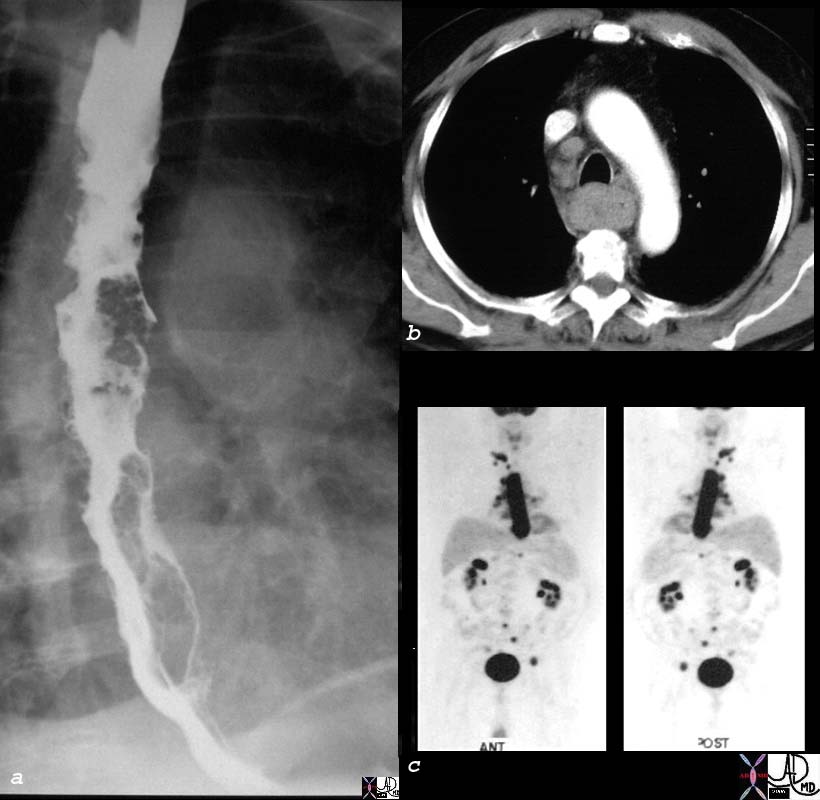 Staging by Non Invasive Method
Staging by Non Invasive Method Stent in the Distal Esophagus
Stent in the Distal Esophagus